THE HISTORY OF P.T.S.D.: 5,000 B.C. TO AFGHANISTAN
- Oct 4, 2024
- 85 min read
B.C.
India (5,000 B.C.)
India (5,000 B.C.) Samba dressed as a pregnant woman, presented to the sages - Illustrations from the Barddhaman edition of Mahabharata.
In Western literature, the oldest description of symptoms of PTSD, an anxiety group of disorder, is seen in Homer’s Iliad, written around 720 BC. According to Shay, Achilles was suffering from symptoms of PTSD. However, in the Indian literature, it was mentioned around 5000 BC.
The Mahabharata is a compilation of Indian epics describing symptoms similar to soldiers fighting wars almost 5,000 years ago. Stories from the Buddhist Jakarta record the story of a monk suffering frightful mental images and emotional numbing.
Assyria (3200 B.C.)
The Assyrians left very detailed accounts of their military conquests and battles, according to 2015 study.
Some of these texts were medical texts, which document the traumata and injuries that Assyrian soldiers suffered during these campaigns even though they were protected by various forms of shields, helmets, and armor made from iron scales, a technology that reached its highest level of effectiveness in the Assyrian period. Unfortunately, offensive weapons had also reached their highest level of effectiveness in that period.
Mark Miller has written about the earliest records that address combat trauma dating to ca. 3200 B.C. (“Weapons and tactics change, but P.T.S.D. goes back millennia”). In ancient Uruk (Iraq), the Assyrians were the first to make cuneiform impressions of their military campaigns and battles. I will give a small sampling of what archaeologists discovered among the 500,000
Middle Assyrian Cuneiform tablet. administrative memorandum.
“If his words are unintelligible for three days [...] his mouth [F...] and he experiences wandering about for three days in a row F...1.”
“He experiences wandering about (for three) consecutive (days)”; this means: “he experiences alteration of mentation (for three) consecutive (days).”
“If his words are unintelligible and depression keeps falling on him at regular intervals (and he has been sick) for three days F...]”
Assyria (3200 B.C.)
Audience scene with procession of horses, soldiers, chariots, dignitaries and eunuchs (section). Wall painting from the Neo Assyrian palace at Tell Ahmar, ancient Til-Barsip (or Kar-Salmanazar), room XXIV, VIII century BC. 1/1 scale facsimile by Lucien Cavro, reproduced at the Louvre Museum.
Another Assyrian warrior received a diagnosis from an ašipu (ashipu) “doctor” recorded on clay tablets:
“in the evening, he sees either a living person or a dead person or someone known to him or someone not known to him or anybody or anything and becomes afraid; he turns around but, like one who has [been hexed with?] rancid oil, his mouth is seized so that he is unable to cry out to one who sleeps next to him, ‘hand’ of ghost (var. hand of [...]).”
“[If ] his mentation is altered so that he is not in full possession of his faculties, ‘hand’ of a roving ghost; he will die.”24
“ . . . but, like one who has [been hexed with?] rancid oil, his mouth is seized so that he is unable to cry out to one who sleeps next to him, ‘hand’ of ghost (var. hand of […]).”
Egypt (1900 B.C.)
Drs. Sethanne Howard and Mark W. Crandall have described an Egyptian physician around 1900 B.C. who had quite a visceral reaction to his trauma. Hori wrote, “You determine to go forward. . . . Shuddering seizes you, the hair on your head stands on end, your soul lies in your hand.” PTSD? Something happened to cause him to feel as he did.
Egypt (1900 B.C.) Warriors figures ushabtis.
Greece
Homer (850 B.C.) )
In book XXIV of Homer’s Iliad, written about 850 B.C., Achilles becomes prey to recollections about his friend Patroclus, who is killed in combat (book XVI). These recollections are recurrent and. cause very disturbed sleep (Homer, 1950):
“But Achilles went on grieving for his friend, whom he could not banish from his mind, and all-conquering sleep refused to visit him. He tossed to one side and the other, thinking always of his loss, of Patroclus’ manliness and spirit... of fights with the enemy and adventures on unfriendly seas. As memories crowded in on him, the warm tears poured down his cheeks.”
Greece 850 B.C. The Illiad of Homer.
Hippocrates (460–370 B.C.)
Hippocrates describes two female patients who displayed symptoms of PTSD. He noted the first woman’s fear, depression, and incoherent speech. The second woman was mute, fumbling, plucking, and scratching. She pulled her hair out, laughed, and wept, all without speaking. At the battle of Marathon in 490 B.C., we discover Epizelus, an Athenian soldier and the son of Cuphagoras.
Facsimile of a bust of Hippocrates.
In battle, Herodotus recorded this fearless warrior was struck with total blindness, which lasted the remainder of his life. Epizelus believed he saw a giant, bearded warrior who, instead of killing him, slew the man next to Epizelus. PTSD? In his research spanning the centuries from Thermopylae to Hue and the Tet Offensive of 1968, Stephen Bentley tells us that soldiers have always had a disturbing reaction to combat.
Alexander the Great (356–323 B.C.)
Plutarch recorded in his The Lives of the Noble Grecians and Romans at 22, 2 years after his father was assassinated in 336 B.C., Alexander crossed the Hellespont with an army of just over 30,000 men to conquer the “known” world. In 10 years of bloody hand-to-hand combat, in which he received several near-fatal wounds and saw legions of comrades struck down by injury and disease, Alexander subjugated the vast Persian Empire of Darius III to become “Lord of Asia.” However, when he reached western India, his exhausted troops refused to march further, forcing him to halt his conquest to the east and return to his new capital at Babylon. Although until that time, he had been a peerless leader, brave, adventurous, adaptable, ingenious, and considerate of those who served under him, Alexander began to exhibit disturbing changes in his character during his return from India. First, he drove his exhausted army through the Gadrosian Desert, where two-thirds perished from dehydration, starvation, and hyperthermia. Then, he began executing the lieutenants and satraps who had served him as middle managers of the empire during his conquests to the east. By the time he reached Babylon, he was drinking heavily. He had become so pathologically suspicious and easily alarmed that he regarded the “least unusual or extraordinary thing as a prodigy or a presage.” During one of his alcoholic binges, he developed a mysterious febrile illness that killed him and ended plans then formulated for renewed conquest around the Arabian peninsula and across North Africa.
Alexander the Great mosaic.in the British Museum.
E. Badian, in his book Studies in Greek and Roman History, found that Alexander lost interest in things he used to enjoy. He felt distant and cut off from people. Falling or staying asleep, irritability, or angry outbursts troubled him. In Alexander’s case, because of his nearly constant drunkenness for at least seven months before he died, alcohol dependence rather than P.T.S.D. has to be considered the principal diagnosis. It is also possible that after more than a decade of fighting, scheming, and murdering in pursuit of absolute power, Alexander changed because he realized that absolute power demanded eternal vigilance.
Appian (149 B.C.)
Appian describes the sack of Carthage (149 B.C.), which must have been brutal and prolonged. The commander, Scipio, recognizing the strain under which his soldiers fought, took appropriate steps to protect them emotionally. In a long passage, Appian writes about the gruesome hand-to-hand warfare of street fighting. “Six days and nights were consumed in this kind of fighting, the soldiers being changed so that they might not be worn out with toil, slaughter, want of sleep, and these horrid sights” (Punic Wars, 130).
In 1868 Poynter produced another of his most celebrated Roman spectaculars, The Catapult. This shows Roman soldiers manning a siege engine for an attack on the walls of Carthage, during the siege which ended in the destruction of Carthage in 146 BC. The famous command of Cato the Elder, "Delenda est Carthago" (quoted in Pultarch's "Life of Cato") is carved in the wood of the huge catapult. The picture was a great success.
Plutarch
(Creative Commons Attribution-Share Alike 3.0 Unported license.)
Life of Marius 45:
But Marius himself, now worn out with toils, deluged, as it were, with anxieties, and wearied, could not sustain his spirits, which shook within him as he again faced the overpowering thought of a new war, of fresh struggles, of terrors known by experience to be dreadful, and of utter weariness.
. . . Tortured by such reflections, and bringing into review his long wandering, his flights, and his perils, as he was driven over land and sea, he fell into a state of dreadful despair, and was a prey to nightly terrors and harassing dreams. . . . And since above all things he dreaded the sleepless nights, he gave himself up to drinking-bouts and drunkenness at unseasonable hours and in a manner unsuited to his years, trying thus to induce sleep as a way of escape from his anxious thoughts.
Lucretius (98–55 BC)
Lucretius wrote specifically about battle dreams, nightmares, and traumatic dreams in one of his philosophical works, De Natura Rerum,
Whatever employment has the strongest hold on our interest or has last filled our waking hours, to engage the mind’s attention, that is what seems most often to keep us occupied in dreams. . . . Generals lead their troops into action. Sailors continue their pitched battle with the winds.
Illustration of a seal bearing the head of Titus Lucretius Carus (about 94-55 BC), better known as just Lucretius. He was a Roman poet who is best known for his poem De Rerum Natura (The Nature of Things), which was written in six books.
Very similar to a rule is the behavior in the sleep of human minds, whose mighty machinations produce massive feats. Kings take cities by storm, are themselves taken captive, join in the battle and cry aloud as though their throats were being slit — and all without stirring from the spot.
A fragmentary inscription commemorated the life of the soldier Ulpius Optatus (CIL 8, 21562). It links ancient soldiers to combat stress. There are two halves of the inscription. The first half recalls Optatus’s bravery and mastery in fighting Rome’s enemies. The second part of the inscription interests them most. Optatus reached a point in the battle when his mind fractured somehow. The wording states, “as he unleashed his excessive anger in its entirety, that familiar rage of battle.” Many ancient and modern soldiers often reached hyper-arousal, or a ‘berserk’ state, suggesting P.T.S.D.
A.D.
Alderman Elfrick A.D. 1003
In the first millennium after the birth of Christ, in 1003, the English were battling the Danes. The English commander, Alderman Elfrick, apparently became violently ill so that he could no longer lead his men. His vomiting was perhaps the onset of P.T.S.D., in Part 3 of A.D. 920 -1014, “Online Medieval and Classical Library Release #17.”
14th Century A.D. Jean Froissart
Half-length portrait of Jean Froissart, historian, facing to the right. Engraved by Nicolas de Larmessin. Isaac Bullart. Académie Des Sciences Et Des Arts. - Amsterdam: Elzevier, 1682.
“Jean Froissart (1337?-1400/01) was the most representative chronicler of the Hundred Years’ War between England and France.” In 1388, Froissart lived at the court of Gaston Phoebus, Comte de Foix. He wrote of the case of the Comte’s brother, Pierre de Beam. Pierre would not sleep near his wife and children since he was in the habit of waking at night, taking hold of a “sword to fight oneiric enemies.”
Soldiers coming fully awake while having frightening dreams in which they reexperienced battles in their past is common in classical literature, as, “for instance, Mercutio’s account of Queen Mab in Shakespeare's Romeo and Juliet (I, iv):
Sometime she driveth o’er a soldier’s neck.
And then dreams he of cutting foreign throats.
Of breaches, ambuscadoes, Spanish blades,
Of healths five fathom deep; and then anon
Drums in his ear, at which he starts and wakes,
And being thus frighted, swears a prayer or two,
And sleeps again.
1666 The Great London Fire (see Illustration 12, p. 117)
According to Stephen Bentley, the Great London Fire of 1666 produced many P.T.S.D.-like symptoms in the population. It was a devastating conflagration that killed many and permanently brought deep suffering to the people of London. John Evelyn’s Journal of the Great London Fire of 1666 records the following:
'The Great Fire of London 1666'. The City is depicted on September 4th, the third day of the fire. Robert Hooke was in London at the time. Fortunately, the fire did not reach his rooms at Gresham College. Such terrifying destruction is on a par with the firestorms after World War II bombings. The narrow streets, timber-framed, thatched houses would later be replaced by brick, stone and tiled buildings to prevent such a tragedy happening again. Oil on board. Rita Greer 2008.
The conflagration was so universal, and the people so astonished, that from the beginning, I know not by what despondency or fate, but crying out and lamentation, running about like distracted creatures without at all attempting to save even their goods; such strange consternation there was among them.
Samuel Pepys personally described the fire in such terrible terms: “. . . and between churches and houses, as far as we could see up the hill of the City, in a most horrid malicious bloody flame, not like the fine flame of an ordinary fire.”. . . So great was our fear, . . . I . . . saw the saddest sight of desolation that I ever saw; everywhere great fires, oyle-cellars, and brimstone, and other things burning. I became afeard to stay there long, and therefore down again as fast as I could, the fire being spread as far as I could see it; . . . how horridly the sky looks, all on a fire in the night, was enough to put us out of our wits; and, indeed, it was extremely dreadful, for it looks just as if it was at us; and the whole heaven on fire. . . . and there saw it all on fire, . . . and the fire with extraordinary vehemence. . . . and such fear of fire in my heart, that I took little rest.”
Two weeks later, Pepys wrote that he is “[M]uch terrified in the nights nowadays, with dreams of fire and falling down of houses.” The diary reports general feelings of anger and discontent over the next four months. Pepys then records that news of a chimney fire some distance away “put me into much fear and trouble. . . . At last [I] met my Lord Mayor in Cannon Street, like a man spent, with a [handkerchief] about his neck. To the King’s message, he cried, like a fainting woman, ‘Lord, what can I do? I am spent: people will not obey me. I have been pulling down houses, but the fire overtakes us faster than we can do it.’. . . So he left me, and I him, and walked home; seeing people all distracted, and no manner of means
used to quench the fire.”
1678 European Doctors
Stephen Bentley has done a massive amount of investigation on P.T.S.D. He tells us that as late as 1678, the Germans, French, and Spanish physicians had already identified the disorder we know today as P.T.S.D. They called it “nostalgia,” defining it by the empirical data, e.g., constant thinking of home, disturbed sleep or insomnia, weakness, loss of appetite, anxiety, cardiac palpitations, stupor, and fever. German doctors referred to P.T.S.D. as “Heimweh,” meaning “homesickness.” The French physicians, noting the same symptoms, called it “Maladie du pays,” and the Spanish termed it “estar roto,” or “to be broken.”
17th and 18th Centuries Doctor Josef Leopold Auenbrugger
In the 17th and 18th centuries, P.T.S.D., although not so named, was very much present during the never-ending wars once gunpowder became readily available. It was thought homesickness among the young troops contributed to the effects evidenced by the day's physicians. One such Austrian doctor, Josef Leopold Auenbrugger, noted P.T.S.D.-like symptoms in the closing days of the Seven Years' War.
August 1768 Capt. Jam
Mackowiak and Batten have done an interesting study on Capt. James Cook was the same Cook we all studied in school. Their article, “Post-Traumatic Stress Reactions,” discovered that from August 1768 to July 1771, Captain Cook’s maiden voyage, Cook recorded that the dangers he and his crew encountered were many:
Captain Cook's original voyages around the world, of his discoveries in geography, navigation, astronomy, &c., with memoirs of his life, and with memoirs of his life, and particulars relative to his unfortunate death.
Cook nearly perished when his ship struck a reef off Australia; he had his first encounter with cannibalism; he lost one-third of his men to a shipboard epidemic of unknown etiology, which also nearly killed him; and, after almost 3 years of the strains and stresses of command at sea, he returned to England to find that a son and daughter had died during his absence.
Not long after returning to England from his first voyage, Cook set about preparing another ship and crew for his second trip, lasting three years, from July 1772 to July 1775. It proved dangerous and demanding on the ship, crew, and especially on Capt. Cook himself. He set sail for Tahiti, sending him near Antarctica. Nearing Tahiti, his ship ran aground on a reef. The Capt. suffered from Gall stones, was wounded in the hand, witnessed cannibalism, and lost one of his Marines at sea. Cook returned to England, finished with the sea, and needed rest.
A year later, in 1776, Capt. Cook set sail on his third voyage against the better judgment of friends and seamen alike. Everyone who knew the captain appreciated him for his good humor, moderation, gentleness, and navigational skills. But something had changed about the captain. He became cruel, irritable, and profane as the ship’s skipper. Indecision invaded his decision-making. He vacillated as to his purpose and plans. Foolhardiness tempted him, as seen by his sailing at full speed into the fog when visibility was 100 yards or less. Against Hawaiian warriors, Cook was killed for no other reason than his provocation toward these islanders, choosing to fight rather than escape. P.T.S.D. Was this combat trauma?
The French and Indian War (a.k.a., The Seven Years War, 1756-1763)
Illustration depicting Braddock's defeat, performed by royal authority.
During the French and Indian War, Stephen Bentley’s research suggests “the symptoms (of P.T.S.D.) were believed to be associated with soldiers’ longing to return home and unrelated to actual battlefield experience.” In his “A Short History of P.T.S.D,” Stephen Bentley noted, “The French surgeon Larrey described the disorder as having three different stages. The first concerns heightened excitement and imagination; the second a period of fever and prominent gastrointestinal symptoms; and the final stage is one of frustration and depression.”
U.S. Revolutionary War (1775–1783)
The Continental Congress authorized one surgeon to serve in each regiment. Unfortunately, and all too often, regimental surgeons received their training through the apprenticeship system. There were only two medical schools in the United States (King’s College [now Columbia University] in New York, NY, and the University of Pennsylvania in Philadelphia, PA). None had any experience treating trauma. The organization was minimal. Moreover, regimental surgeons tended to work for their unit instead of seeing themselves as part of the Hospital Department. Bureaucratic infighting rendered this system ineffective.
Revolutionary War (montage).
As early as 1685 in Philadelphia, the Quaker Society of Friends, following an earlier British law, the English Poor Law of 1601, took responsibility for the poor. The churches and private organizations established assistance for those in need. In England, the local citizenry was to “provide certain maintenance through compulsory taxation when a family was unable to provide for a mentally ill member.” In America, this help included those soldiers whose lives would be radically altered by the country’s revolution against England. “Widows, orphans, and invalids received aid, but only if they could not rely on relatives, friends, or other parties deemed to have responsibility for them.”
Azel Woodworth
Azel Woodworth was only 15 years old when he served at the Battle of Groton Heights in 1781. After enlisting the previous year in Captain William Latham’s matross company, which assisted in loading, firing and sponging guns, Woodworth helped defend Fort Griswold from invading British troops — until a musket ball struck his neck, just under his right ear, and exited along his spine, cutting through skin, muscles, tendons and bone. As Woodworth later recalled, the injury rendered him “insensible” for a “short interval.” Then, he “partially recovered” and resumed military action. The following day, however, his mental “faculties retired” and “returned not for 24 hours.” Woodworth’s wound not only caused his head to permanently rest on his left shoulder, but also significant intellectual incapacity that waxed and waned over the course of his life.
Woodworth’s injuries to his head, neck and intellect dramatically altered the adulthood he had imagined for himself at the age of 15. As he later wrote in a memoir — which was reprinted in William Wallis Harris’s The Battle of Groton Heights: A Collection of Narratives, published in 1870 — due to Woodworth’s “deranged state,” his father stopped teaching him a trade, believing that he would be “unable to progress in the study.” Even manual day labor, which Woodworth pursued as a result, “exhausted” his “mental faculties,” causing him pain and requiring frequent breaks. In the 1790s, the veteran married, had two children, and pursued a business in husbandry. Yet his difficulties in laboring soon led to financial troubles. Despite receiving a small monthly “invalid” pension of $1.66 from the newly formed federal government in 1794, by 1807 Woodworth had become a self-described “wandering person” dependent on the “charity of fortuitous friends.”
Richard Watrous
After Richard Watrous, a private in the Sixth Connecticut Regiment, was wounded in the Battle of Norwalk in 1779, he received intensive and prolonged support from fellow soldiers, doctors, family members and townspeople. Watrous was injured in his arms and torso by musket balls and bayonets, causing fractures and wounds, as well as disturbances to his mental state. As neighbors explained, he “appears to be lost & bewildered” much of the time, perhaps owing to “some radical injury to his constitution.” Watrous was first cared for by servicemen and former neighbors, then by physicians and military officers, and finally by family and community members at home. As one neighbor recalled, an officer “assured me [that Watrous] Should have all Possible Care taken of him,” a support that eased the veteran’s mental and corporeal struggles until his death in 1799.
The War of 1812
Gen. William Hull
The War of 1812 created more mental anguish for those involved directly. Symptoms of P.T.S.D. surfaced following the American Revolution. During the War of 1812, these traits were especially poignant in the life of Gen. William Hull. George Washington had seen Hull’s promotion to General for bravery during the War of Independence just before the Northwest Army’s devastating defeat at the Battle of Detroit. Gen. Hull was tried and convicted of cowardice, but President Madison commuted his sentence.
Gen. William Hull. Artist: James Sharples Sr. (1751-1811).
Hull, the hero of Saratoga and Monmouth’s battles, probably suffered P.T.S.D. to a much higher degree than was reported until the battle of Detroit. According to Joseph R. Miller, in “War and Trauma: The Dual Life of William Hull,” Hull’s daughter wrote of her father’s heroics:
It is sufficient for my purpose on this occasion, to notice particularly the capture of Burgoyne (Saratoga), and the well-known battle of Monmouth. In these two memorable events, where the ground was covered with the dead bodies of the slain, and the air resounded with the groans of the dying, Hull was unshaken. He bravely fought, and a grateful country acknowledged his bravery . . . . Having associated with him in times so interesting, and in no other character than that of a brave man, I shall be unhappy to learn that he has terminated his patriotic career by meanly acting the coward.
Charles Dickens (1812 – 1870)
Charles Dickens noted the symptoms he experienced after a train crash where ten people died and hurt as many as 49. He wrote, “I am curiously weak. . . I begin to feel it more in my head. . . but I write half a dozen notes, and turn faint and ‘‘sick’’. . . driving into Rochester yesterday I felt more shaken ‘‘than I have since the accident.’’ ‘‘I cannot bear railway traveling yet.” Charles Dickens wrote A Tale of Two Cities, which (published in 1859) can be considered as an early case report of PTSD" (Huber and te Wildt, 2005).
French neurologist Pierre Janet (1859–1947) (see Illustration 19, p. 119)
The French neurologist Pierre Janet (1859–1947) was one of the first scientists to empirically explore trauma’s psychological impact. In a study of more than 5000 patients, he suggested that traumatic memories have the ‘all or none’ feature. He also concluded that trauma is often decontextualized and misplaced in its historical context.
Creative Commons Attribution 4.0.
Janet recognized what he called ‘premeditation,’ when a person experienced a traumatic event and when the patient developed trauma-related symptoms. If the victim re-experienced a particularly traumatic event, Janet called this a dissociative flashback. Patients were incapable of processing the memories of a traumatic event.
Janet describes the concept of
‘misere psychologique,’ a degrading of the psychic functioning particularly observable in the wake of emotionally draining traumatic experiences.
1884
German physician Hermann Oppenheim first coined the term “traumatic neurosis.” Oppenheim described 42 cases of “railway or workplace accidents.” Charcot would have none of it. He insisted that “these cases were only forms of hysteria, neurasthenia, or hystero-neurasthenia.”
But after Charcot died, the French psychiatry adopted the term “traumatic neurosis.” The Belgian Jean Crocq reported 28 cases of railroad crashes, men and women who suffered from this neurosis. Symptoms included “dissociation caused by trauma, the pathogenic role of forgotten memories, and ‘cathartic’ treatment.”
Emily Dickinson December 10, 1830 - May 15, 1886
Emily Dickinson spent her entire life in Amherst, Massachusetts, sheltered from the outside world among her socially prominent family. As a child, she was “one of the wittiest girls in [her] school, a self-proclaimed free spirit,” and by the time she reached her middle teens, she was brimming with self-confidence, exclaiming, “I am growing handsome very fast indeed! I expect I shall be the belle of Amherst when I reach my 17th year. I don’t doubt that I shall have perfect crowds of admirers at that age.”
At the tender age of 14, four of her closest companions died unexpectedly, one following the other. Emily had little choice but to attend each funeral. “One of these deaths was that of a cousin of the same age, Sophia Holland, into whose room Dickinson stole moments after the girl died.” In her great distress, she could but stare into her late cousin’s peaceful face, transfixed, “until others pulled her away.” Simultaneously, Emily experienced a fever and then a cough that produced blood. This sickness continued for decades, so when she was 17, she quietly canceled her classes and resigned as a student at Mount Holyoke College. Miss Dickenson’s family had suffered from this disorder, and therefore, it was supposed to be hereditary.
Even though she became her mother’s primary caregiver, Dickinson secluded herself from almost all social contact by the late 1850s. She no longer wished to gather with close friends. Her church attendance waned and then became nonexistent. When guests approached, Emily would beat a hasty retreat. She developed an odd method of tolerating visitors. She agreed to converse with guests only at moonlight and then at her home’s back stairs. All her conversations came from behind a door or screen. Her doctor was allowed to examine her oddly. He would seat himself at the far end of the room, and as she walked by the open, he must make his prognosis. By age 35, her recovery seemed more assured. It was then she ventured outward into her social surroundings. At this time, her poems and essays began to blossom, and she became the writer we know today. “She died at age 56, most likely of hypertension complicated by a massive stroke.”
The Crimean War October 1853 - February 1856
During this war, “Irritable Heart” had been recorded, resulting in the incapacitation of soldiers. Light duty and rest were prescribed. “Many years after the end of the Crimean War, traumatized veterans are recognized as suffering from Da Costa syndrome or Effort syndrome, although neither name is used until long after the war.”
"Print shows soldiers transporting winter clothing, lumber for huts, and other supplies through a snow-covered landscape, with partially buried dead horses along the roadside, to the British camps; huts under construction in the background." tinted lithograph, digitized from the original print. Simpson, William, 1823-1899, artist., Paul & Dominic Colnaghi & Co., publishers.
The Attack on the Malakoff by w:William Simpson. Print shows the French assault on the Malakoff, the main Russian fortification before Sevastopolʹ, on 7 September 1855. French soldiers advance from the left, Zouaves from the left foreground, crossing the ditch and engaging. 23. The Crimean War Russian soldiers in hand-to-hand combat on the right. This was published on 22 October 1855, less than two months after the battle, which is about as contemporary to the event as mass-reproduced colour images got at the time.
The horrific suffering endured by the British troops in the Crimean War lacked the dignity and bat- battlefield honor afforded by Lord Tennyson’s poetic stoicism in “The Charge of the Light Brigade.” For of the approximately 20,000 British troops that died in the East, in a vain attempt to settle the “Eastern Question” of what was to become of the Ottoman Empire, only 10 percent were killed in action. Although thousands of Germans, Swiss, and Italians fought for the British Army, most of the British military was composed of fellow compatriots. However, death was no respecter of persons as the vast majority of British military casualties unceremoniously and needlessly succumbed to a varietyof factors afar from the battlefields.
Britain went to war ill-prepared medically or administratively. Army Medical Department Director-General Andrew Smith and his staff had no experience at war or preparing for it. However, by the conclusion of hostilities, Smith had published a beneficial work titled Medico-Chirurgical History of the War. The British Department of War Office published Smith’s work. The first volume was the “Precis,” which the War Office divided into two parts. The War Office further divided the second volume. This book, Medical and Surgical History of the British Army, which Served in Turkey and the Crimea during the War Against Russia in the Years 1854-55-56, became an essential part of British medical treatment. “(W)hen taken in its totality, the value of the publication is undeniable and provides insight into the overall health of the British military and the spectrum of maladies troops endured during the Crimean War.”
For of the approximately 20,000 British troops that died in the East, in a vain attempt to settle the “Eastern Question” of what was to become of the Ottoman Empire, only 10 percent were killed in action.
Of the “34,318 troops were deployed in the Crimea,” by June 3, 1855, roughly 48,039 served in Crimea. “By the end of March of 1856, and the Treaty of Paris signing, 111,313 British officers and soldiers had made it to the theater.” Statistics revealed “2,755 were killed in action and 2,019 died of wounds.” Officially, though, “the British government recorded a total of 21,097 deaths in the Crimean; thus 16,323 died of diseases.”
“It is difficult to recognise in their haggard faces and ragged clothing the gay soldiers who left us the other day. Every general and staff officer in our division was killed or wounded. The people who are left appear dazed and stupefied and unable to give us any idea of our position or chances.” -Lieutenant Llewellyn.
Long after hostilities ended in Crimea, “traumatized veterans are recognized as suffering from Da Costa syndrome or Effort syndrome, although neither name is used until long after the war.”
Florence Nightingale (1820–1910)
Florence Nightingale was a remarkable and religious woman, born into an aristocratic British family. Her parents educated her at home. Although frail, Florence was exceptionally independent and thoughtful. She grew into womanhood when British women had few rights, and the society passed over females of insight and intellect like Florence.
Nightingale had the courage and conviction to challenge her society’s strictures and take up the then-masculine vocation of nursing. In 1854, in her middle thirties, she traveled to Skutari (now Uskudar), Turkey, to care for British soldiers fighting the Russians in the Crimea. With a mere 38 nurses under her, she provided medical care to a seemingly endless stream of troops wracked by frostbite, gangrene, dysentery, and other diseases and crammed into 4 miles of beds not 18 inches apart.
Days came in endless cycles, seeing her nurse patients up to “20 hours a day.” Florence “took the most severe cases herself.” The following May, Florence was diagnosed with what was most likely brucellosis, a near-fatal illness. Weak and sick as she was, Nightingale refused evacuation back to England.
Nightingale’s work brought the field of public health to national attention. She was one of the first in Europe to grasp the principles of the new science of statistics and to apply them to military—and later civilian—hospitals. 1907 she was the first woman to be awarded the Order of Merit. Nightingale’s image has often been sentimentalized as the epitome of femininity, but she is especially remarkable for her intelligence, determination, and amazing capacity for work.
She remained with the Army during her convalescence and did not leave her post until the last soldier had left for home 21 months after her arrival.” Her nursing in such Spartan conditions, living among the dead and dying had hardened her, and she was visibly aged by her serious illness and resulting exhaustion. Intermittent fevers, anorexia, fatigue, insomnia, irritability, depression, sciatica, dyspnea, and palpitations dogged her for the next thirty years. Miss Nightingale seldom left her sofa and confined herself to her room.
Her memories haunted Florence of those who died after she attempted to nurse them. She was a “bereaved, haunted woman” who walked her room during the night, unable to sleep. It was not until into her sixties that her troubles began to subside. She had become a “cold, obsessed, and tyrannical workaholic.” Her more positive transformation came late in life, albeit gradually. The mental hardness produced by her medical activities during the Crimean War had softened, and Florence showed hopeful signs of life. She even began pursuing more normal relations with old friends. After attending to her last patient, Scutari had long since eroded the nursing desire. Miss Nightingale died of “old age and heart failure” at age 90.
Suicides
Director-General Andrew Smith cataloged “suicides” as death by “disease.” Eighteen “diseased” soldiers officially took their own lives. “Attempting to calculate an accurate annual suicide rate per 100,000 is impossible because it is unclear how many of the 111,313 military personnel arrived in-country for the basic two years of the war, but the range is conservatively between 8 and 16 per 100,000, with the likely answer somewhere near the middle.” Interesting is the fact that of these 18 suicides, all but two suicides served in different regiments. Medical staff documented fifteen of the 18 suicides as “Died in General Hospitals and elsewhere (not in Regimental Hospitals) during the War.”
The American Civil War 1860 - 1865
Death of General Thomas Williams at the Battle of Baton Rouge, illustration by Harper's Pictorial History of the Civil War, Volume 2.
The first understanding that a traumatic event could cause psychological as well as physical injury. People traumatized by accidents on railways were referred to as having Railroad Spinal Syndrome by the English surgeon Frederick Erichsen.
Before the Civil War, there were no national cemeteries and no governmental procedure for even identifying the bodies of men lost in battle, much less for burying them. The nation had no “bureaucracy” of death simply because there had been no need for it. At first, most people saw the war as a minor contretemps or dispute. At the capture of Ft. Sumter in April 1861, no one expected it to last very long. Between April 12, 1861, and June 30, 1861, both sides suffered 30 casualties: four Union and 26 Confederate.
It is essential to understand how Americans looked at death before the war since that view is so alien to many of us now. Of course, death is always a part of life. The prevailing belief about death in the early decades of the republic was that the subject itself had become a prominent feature of the country’s mental landscape. This philosophy of death guided a person’s life. An omnipresent goal of having a “good death” meant dying at home. The departed had uttered his or her last words surrounded by loved ones.
Illustration by Harper's Pictorial History of the Civil War, Volume 2.
During the war, a soldier wounded in battle, far from home, and about to die would often arrange photographs of family members around him. In this way, the soldier attempted a rudimentary battlefield version of the once-idealized good death at home. After June 30, 1861, this “good death” changed radically. During the Civil War, identifying the dead proved distressing to the men’s units and the family members waiting at home for some word from their relatives fighting in the war. In part, that was because of crude battlefield burials, if there were burials at all. The contempt each side eventually had for the other’s death was the cause. At Antietam, northern soldiers dumped 58 dead rebels into a well.
For the first time in modern history, war technology has outstripped man’s ability to cope. Men had raced headlong into their enemy’s ranks for millennia, facing spears and arrows. In the Civil War, the combatants faced repeating rifles and Gatling guns, delayed fuse artillery rounds that burst in mid-air, killing tens of hundreds of soldiers before they could get close enough to close with the enemy. No generation had faced telescopic sights and rifled bores that could reach out and strike men dead hundreds of yards away. The soldier did not have to participate in the battle to face exposure from a sniper too far away to see.
From 15% to 20% of the Union Army soldiers enlisted as volunteers between 9 and 17. Ninety-three percent of the men would likely “experience mental and physical disease.” Soldiers and POWs alike fell victim to “cardiovascular disease, gastrointestinal symptoms, and would probably die “early.” Beyond the death and destruction of the war itself, many in the Union Army had relatives in the Rebel Army. “Family members” participated in trying to kill each other in close-quarter, hand-to-hand combat, with devastating consequences. This type of warfare caused tremendous distress not only because of the physical carnage but also because killing one’s kin at close range presented mental psychosis.
Daniel Folsom
Daniel Folsom, a tinsmith from northern New York, enlisted in the Union Army just days after the fall of Fort Sumter. His exemplary service through years of long marches and hard battles led to two promotions, but something changed during the Battle of Fredericksburg in late 1862. Folsom seemed un-easy. He was still troubled months later when the regiment mustered out. He returned home, opened his tin shop, and tried to focus on work.
As time passed, Folsom’s motivation to work waned. He neglected the tin shop and wandered aimlessly around the village. Folsom snapped in July 1863 when the draft called the first men in his neighborhood. Terrified that he would be sent back to the Army, he became sleepless and manic and then fell into a severe depression. When he attempted suicide, his family had him committed to the State Lunatic Asylum in Utica. In the asylum, the young veteran grappled with his paranoia and guilt. At times, he begged the attendants to kill him.
Folsom slowly began to improve. “I am not injoying myself much at present,” he wrote to his sister in the spring of 1864. Still, he assured her he had recovered and implored her to persuade their father to retrieve him from the asylum. Folsom was especially concerned about finding work. It seemed to him that the longer he was institutionalized, the less likely it would be for him to succeed in business. “I should like to get out of this city [and] go into business if I stay here any longer the world will be a blank,” he wrote. “I think there is a chance for me yet."
Wallace Woodford - Once back in the safety of his bed, “Wallace Woodford flailed in his sleep, dreaming that he was still searching for food at Andersonville. He perished at age 22, and his family buried him beneath a headstone that reads: ‘8 months a sufferer in Rebel prison; He came home to die.’”
Those soldiers diagnosed as “insane” from the exposure and rigors of battle would often wander about the countryside. Some died utterly unaware of the new dangers they faced. Many of these once brave but later broken men existed for years afterward and eventually committed suicide. Others spent their final days in insane asylums. Unfortunately, the government did little to maintain the hospital they had built for the Insane in 1863. Soldiers’ homes sprang up throughout the nation after the war, their need growing with the ensuing years rather than decreasing.
On November 11, 2014, HBO aired a documentary titled Wartorn 1861-2010, a film about combat trauma from the Civil War to Iraq and Afghanistan’s current involvement. Directors Jon Alpert and Ellen Goosenberg Kent found it difficult to locate and document information on Civil War veterans and their combat stress claims. Legal pension files recorded the families of the veteran’s descriptions of their loved ones who had returned home mentally altered. Often, the breadwinner could no longer function psychologically. From those files, individual tales revealed what the war had done to these men.
Brigadier General Philip St. George Cocke - Writing for the New York Times, Sommerville records. the suicide of the highest-ranking Confederate officer, Brigadier General Philip St. George Cocke. Due to losing his command and rank as the “appointed commander of Virginia’s state forces” once the war started, his superiors demoted him to Colonel. However, he regained his Brigadier General’s rank at the first battle of Bull Run, but his brain had suffered irreparable damage.
He commanded troops in the Battle of Blackburn's Ford and the First Battle of Bull Run
(First Manassas) in July 1861.
Psychologically and physically, these “perceived slights, on top of the strain of war, combined to take a huge toll on Cocke’s psychological and physical health. He retreated to his plantation a broken man, and on the day after Christmas 1861, he shot himself in the head with a pistol.” (see Illustrations 27, p. 122)
Suicide Rates During and After the Civil War
Hadley-Cousins gives some rather disturbing statistics from an official report by “The Medical and Surgical History of the War of the Rebellion.” Eight hundred fifty-three soldiers were discharged for insanity, 1% of the total post-war discharges. That number is probably relatively low, considering the number of battles, the casualties, and the types of wounds sustained from five years of war. We are only made aware of the mental instabilities from the remaining asylum records. For men like Daniel Folsom, who believed he “still had a chance” and “I shall try and be a man,” as he wrote home later, reenlisting in the army helped “to reaffirm his manhood through battle.” Folsom survived the war as a 1st Lieutenant with a New York regiment, living to marry and produce six daughters.
Dr. Jacob Mendez Da Costa - Following the U.S. Civil War, doctors began to notice an increase in troops’ heart problems, attributed to fatigue from war conditions. Doctors treated fatigue, anxiety, high blood pressure, and irritable heart conditions with rest.
Sketch for Portrait of Dr. Jacob Mendez da Costa by Thomas Eakins.
In 1871, Dr. Jacob Mendez Da Costa converted the term “nostalgia” to “soldiers' heart” after noticing increased heart problems among soldiers and civilians. He attributed the symptoms to fatigue caused by excessive marching, complex service in the field, and missing loved ones. The recommended treatment for soldiers’ heart also consisted of rest. “Instances of sudden paralysis or loss of sensation were identified as traumatic hysterical neurosis.”
In 1981, M. R. Trimble reviewed case studies of railway accident survivors of the 1700s. These produced head injuries that Trimble traced. There appeared to be biological components that created PTSD-like symptoms. These indications gave rise to the term “postconcussion syndrome.”
According to Trimble, the English surgeon Erichsen attributed conspicuous psychological abnormalities following railway accidents to microtraumas of the spinal cord, which led to the concept of the “railroad spine syndrome.” This original connection drawn by Erichsen was later contradicted by the surgeon Page (1885), who objected to the phrase “concussion of the spine.”
Page believed that injuries to the spinal cord could produce emotions such as fright, fear, and alarm, contributing to the disorder. He suggested terms more aligned with the responses, e.g., “nerve shock” and “functional disorders.” Although Page argued that nervous shock is more psychological in nature and origin, the nervous system’s physiologic malfunction often results. In 1883, Putnam maintained that many of these cases, known as railroad spine syndrome, should better be associated with hysterical neuroses. Hermann Oppenheim first spoke of trauma and traumatic neurosis, a disorder he located in the cerebrum. Until that time, it referred almost exclusively to surgery. Suddenly, trauma could also deal with psychiatry.
The available data, then, scanty at best, would not support the assumed pathology of the spinal cord or heart disease. The question arose as to the interpretation of trauma for post-traumatic syndromes. External factors deduced from psychoanalytic understanding were quickly adopted as having significant weight in diagnosis. (see Illustrations 28, p. 122)
The History of P.T.S.D.: Post Civil War to WWII
Post Civil War
W. C. MacLean conducted an 1865 study at the Army Medical School in Netley, England. MacLean based his report on a previous Crimean War investigation by de Costa on soldiers’ equipment. The study suggested the equipment needed a redesign. The government issued rucksacks and waist belts that ‘were thought to restrict circulation through the heart, lungs, and great vessels.’ In well-disciplined regiments, the practice of falling out at drill or on the line of march is discouraged, and [that] men will bear and suffer much, rather than incur the imputation of being ‘soft.’”
In 1871, Jacob Mendez Da Costa published a study on “irritable heart.” Determined military doctors attempted to isolate the growing caseload of “heart disorders” that there “was actually an organic response to battle stress.” In 1873, the U.S. Congress passed the Consolidation Act, rating disabilities for various levels of impairment during the Civil War, according to Blanck and the Bradley Commission of 1956. If a veteran could prove that his disability was caused by his military service, even though such action originated from combat, his present disability was deemed pensionable. Unfortunately, corruption in the disability process increased until the print media published stories verifying “exaggerated and faked claims of disability.”
De Costa reported in 1919 that 38.5% of his 200 psychological disorder patients endured “hard field service and excessive marching.” This meant, according to Meager, they lived under constant threat of death or dismemberment. In that same report, 30.5 % had bouts with diarrhea.
Eighteen eighty-eight brought a Commission of Pensions report to Congress detailing its findings. From 1862 through mid-1888, revealed that a greater number of awards were granted for delayed-onset diseases than for service-incurred injuries. Among the Commission’s reported statistics were 5,320 pensions for nervous prostration and 1,098 pensions for “disease of the brain, including insanity.” An astounding 25,994 cases of “diseases of the heart” were reported.
The Boer War October 11, 1899 – May 31, 1902
Doctors diagnosed and documented functional disorders during the Boer War, making the death certificates more understandable but not necessarily more accurate. Traumatic stress death certificates read, “Disordered action of the heart” or “valvular diseases of the heart.” “The South African War (1899–1902), for example, saw large numbers of British servicemen discharged from the armed forces with a diagnosis of disordered action of the heart (DAH), thought to be the effect of exertion on a soldier’s chest constricted by tight webbing and equipment.” Some soldiers showed symptoms that resembled Gulf War Syndrome. A civil surgeon, Anthony Bowlby (1855–1929), worked at the Portland Hospital in Rondebosch and Bloemfontein in 1900. Bowlby recalled the symptoms he saw in his patients, which included “pain, in the form of headache, generally posterior, pains in the neck, pains in the back and limbs so that these cases are generally sent back as cases of rheumatism; general feebleness of the muscular system amounting to paralysis more or less pronounced.” Seventy-seven percent of British soldiers saw action during this conflict instead of 19% of Gulf War soldiers.
Clockwise from left:
Boers in action at the Battle of Colenso, the 17th Lancers holding of an attack at Modderfontein, General Redvers Buller entering Ladysmith on 27 Feb 1900, Boers at the besieged city of Mafeking, Canadian Troops during the Battle of Paardeberg, and Boers before action at Spion Kop.
Troops who fought in the Boer War often had to march considerable distances to engage the enemy; it was a war of movement without mechanization. Contemporaries believed that the physical exertion involved was, in part, responsible for the various heart disorders encountered. Similarly, shell shock was framed in terms of trench warfare: an expression of the terror felt by men forced to endure the effects of artillery bombardment often without adequate protection and in identifiable positions. Fifty-nine per cent of wounds inflicted on British soldiers were as a result of artillery, and three times as many men were killed by shells as by bullets.
Australian civilian medical authorities during the late nineteenth century believed insanity as a sign of moral weakness. This view resulted “in a feminized view of mental illness.” Real men didn’t go insane because of combat. Therefore, these men had to be kept away from other hospitalized war veterans and sent to insane asylums. “Mental illness among men posed a threat to this legend (‘idealized masculinity’). The Australian colonies mythologized masculinity. The importance of nation-building and rural industry had amplified the masculine ideal, creating the ‘bush worker’ hero of the Australian outback.”
What created such consternation among physicians and Government officials in Australia and Britain was the caliber of men sent to fight in South Africa. New South Wales sent “thousands of unemployed ‘bush workers’ or rural workers.” Joblessness of these types of men meant, “These troops directly represented the ideal Australian male, but this hyper-masculine image precluded the possibility of psychiatric disorder, whether combat-related or not. The Australian concept of selfhood combined with colonial views of ‘insanity’ meant that military authorities questioned the possibility of combat-related psychological trauma. In other words, the concept of the ‘insane,’ feminized soldier was inconceivable.” Even by the time World War I was in full swing, doctors and Government officials had not linked psychiatry and combat.
Treatment: The Russo-Japanese War (1904-1906)
Japanese soldiers entering a bombed fort to find dead and wounded men. Halftone, c. 1905, after C. M. Sheldon, from photographs.
. . . Russian attempts to diagnose and treat battle shock represent the birth of military psychiatry. The Russians’ major contribution was their recognition of the principle of proximity, or forward treatment. Although it’s believed by most armies today that the Russians were right in treating psychiatric casualties close to the front, with the goal of returning them to the fight, the recorded rate of those who returned to battle suggests the method was not very successful. In actuality, less than 20 percent were able to return to the front.
Russian psychiatrists
The most notable Russian psychiatrist was Avtocratov, who first developed what came to be known as “forward psychiatric treatment.” Russian doctors and military command first noticed Post-battle neuro-sis. Avtocratov ran a 50-bed hospital for treating psychiatric patients at Harbin, Manchuria. The Trans- Siberian Railway was not yet completed, and moving psychiatric patients over rugged terrain and long distances created the need for close-to-the-front treatment. In 1904, doctors treated some 1500 patients. In 1905, that number increased to 2000, precipitating calling in Russia’s Red Cross Society. A German doctor, Honigman, served in this body. It was Honigman who labeled traumatic patients with “war neurosis” [Kriegsneurose] in 1907. Previously, psychosis was called “combat hysteria” and “combat neurasthenia.” Honigman also noticed a similarity between Russian war survivors, and Oppenheim’s re- ported railway crashes.
World War I
A German trench occupied by British Soldiers near the Albert-Bapaume road at Ovillers-la-Boisselle, July 1916 during the Battle of the Somme. The men are from A Company, of the 11th Battalion, The Cheshire Regiment.
By the outbreak of the First World War, doctors diagnosed actual psychiatric patients with weak character. Rather than continue to participate in or witness further wholesale disintegration and slaughter of entire armies in France’s muddy trenches, men often fled their posts. Many soldiers went into hiding. The French Government discovered them and subsequently shot them by firing squad for cowardice and desertion of duty. Of the 117,000 Americans killed, over 200,000 were wounded in action, and almost 160,000 had become psychiatric casualties. The military permanently discharged seventy thousand mental cases from the service.
Shell Shock
During World War I and World War II, psychological trauma was termed “shell shock” and considered to be the result of mortar rounds and artillery shells that continuously bombarded the troops. This phrase became the standard reference to traumatized troops. It was coined by Myers, a British military psychiatrist, in 1915.
Gallipoli 1915. The dead bodies of 36 members of the 11th Battalion Battalion killed during the capture of Leane's Trench.
“Has vivid dreams of war episodes—feels as if sinking down in bed”; “Sleeping well but walks in sleep: has never done this before: dreams of France”; “Insomnia with vivid dreams of fighting”; and “Dreams mainly of dead Germans...Got terribly guilty conscience over having killed Huns.”
Mott wrote a year after the Armistice, describing neurosis, hysteria, and neurasthenia as physical shock and horrifying conditions that could cause fear, which in turn produced an intense effect on the mind. Hysterical symptoms included paralysis, contractions, disordered gait, tremors, and shaking. Neurasthenia symptoms included lassitude (mental weariness), fatigue, weariness, headaches, and particularly vivid and terrifying dreams . . . startle reflex.
Probably over 250,000 men suffered from ‘shell shock’ as result of the First World War. The term was coined in 1915 by medical officer Charles Myers. At the time it was believed to result from a phys- ical injury to the nervous system during a heavy bombardment or shell attack, later it became evident that men who had not been exposed directly to such fire were just as traumatised. This was a new ill- ness that had never been seen before on this scale. The condition was poorly understood medically and psychologically. Take a look at the War Committee Report (WO 32/4748) on the condition to find out more about attitudes towards it just after the war. Today, the condition is known as post- traumatic stress disorder and the treatment and attitude to it are very different.
Neurasthenia
Shell-shocked soldier. Australian Dressing Station,Ypres, 1917. The soldier in the bottom left exhibits a typical sign of shell shock – "the thousand-yard stare."
Two cases of neurasthenia also give details of trench warfare and other injuries. The symptoms of this condition include physical and mental exhaustion with headaches or irritability, which can be linked to depression or emotional stress. Many ‘shell shock’ cases displayed symptoms of neurasthenia. (Catalogue ref: MH106/2101)
Neurasthenia is an ill-defined medical condition characterized by lassitude (mental weariness), fatigue, headache, and irritability, associated chiefly with emotional disturbance. In 1914, thirty-two year old Cpl. A. Xxxxxxxxxxx had served sixteen years in the British military. Xxxxxxxxxxx served with the First Cheshires when he suffered a traumatic injury in France. Captain B. McFarland recorded on September 12, 1914, the following about Cpl. Xxxxxxxx at 4th Northern General Hospital, Lincoln:
He has only four front teeth-top side two molars, bottom side and he could not eat biscuits.
On the 7th last month he was out scouting at 7.30 he got 1½ miles into enemies’ lines by mistake he was on a bicycle & had orders to retire- when ½ way back Germans opened fire on either side of road- this corporal was last man. They put a log in front of bicycle & threw him head over heels into a German trench & two of them took him prisoner to their quarters. At 2.30 their [position] was blown for an attack & the 2 … left him & whilst they were away, through a hole in the hedge behind his trench he scrambled to a barn & then jumping into German trench & ran up it for 100 yards until he saw the telegraph lines of British troops. He then ran across the road, jumped into a trench 2 feet deep and then there were about 50 shots fired at him, then he saw the Bedfords Regiment & reported position of enemy to them. He has been subject to Neurasthenia ever since. He was sent to 14 General Hospital for 4 days & then sent on here.
He is much better, sleeps well & eats well & no pains. He will be fit for furlough in a few days.
Six months later, L/Cpl. J. Xxxxxxx had served for thirteen years with the 2nd Lancs. Fusiliers and subsequently sent to 4th Northern General Hospital, Lincoln, from July 6-9, 1915, suffering what Capt. McFarland diagnosed as Neurasthenia.
On 5th May at Ypres he got a severe attack of Gas Asphyxia & was three hours unconscious, his nerves were bad after that, he had a bad shock in the end of November, a Jack Johnson [type of shell] fell about 10 yards from him. It killed 4 horses, wounded 3 men & killed a civilian. In February three shells fell on the house he was in & the roof fell in on top of him but he was not much hurt. He was sent to Etaples Hospital for 11 days. He was sent then to Rouen. Arrived here 18th June, Complaining of pain in head, his nerves are completely shattered. He has bad teeth they want attending to. Old caries [dental cavities] and decayed teeth want removing and a new plate ordered [dentures]. Rest.
Light diet and bromide mixture.
B. McFarland Captain R.A.M.C.
4th Northern General Hospital
Caught a feverish chill and referred to bed.
Temperature down to normal but still complains of pain in legs and given only milk diet still.
During the First World War, 306 British soldiers were executed for cowardice. “Herbert Morrison, . . . was the youngest soldier in the West India Regiment when he was led in front of the firing squad and gunned down for desertion. A ‘coward’ at just 17. . . . To this day, the Ministry of Defence refuses to give a pardon to the 306, convicted of cowardice, though even in 1914, people knew all about ‘shell shock’ - what the modern world calls Post Traumatic Stress Disorder. . . . The historic shaming of men - and, consequentially, their women and children - happened in other countries too. In France and Germany, men were shot for cowardice and desertion. But in the case of Germany, only 25, not 306. And in both countries, that shame was lifted within a decade of the war's end when official memorials were built.
“Only in Britain do we continue to dishonour the victims of shell shock. The Government’s argument
echoes the one first set out by John Major. He told the Commons that pardoning the ‘deserters’ would be
an insult to those who died honourably on the battlefield and that everyone was tried fairly.”
Military doctors, therefore, had to revise the “weak” or “cowardly” diagnosis. As the need for “volunteers” to fight increased, the gains made by Army doctors in treating mental health veterans were soon revised downward by a simple formula, “predisposition plus stress equals collapse.” In British medical studies during the war, what was known then as “post-emotional etiology” moved to the foreground. Post-concussional etiology (origins) receded somewhat, the latter being considered an honorable organ-ic etiology. Germany emphasized not wanting to return the patient to the battle. Therapy then was to isolate the soldier in a dark environment and then conduct shock treatments. Regardless of using these severe shock treatments, doctors returned patients to duty without being healed.
French soldiers sent to hospitals were often considered malingerers and, when released, were tracked down. One such soldier, Louis Ferdinand Destouches, alias Celine (1894-1961), tells his story in his Voyage au bout de la nuit (Journey to the Edge of Night). After several days of fighting, he recounts Ferdinand has a fit of madness while on leave. In the hospital, he tells the army medics that he has been driven mad by fear. He finds himself in the company of others, psychologically submitting to stringent medical monitoring. After a few days, doctors divided the patients into three categories: the first returned to the front, the second involved transferring these men to a psychiatric hospital, and a firing squad shot the malingerers. Sir Grafton E. Smith and T.H. Pear preferred “war strain” to “shell shock.” Incapacitation of one’s duties did not originate from the concussion of artillery rounds.
Second Lieutenant Bertwistle
. . . with two years of service in the 27th Australian Infantry, although only 20 years of age, whose face wears a “puzzled expression” and who exhibits a “marked defect of recent and remote memory.” “His mental content appears to be puerile. He is docile,” according to the records that accompanied him from the Royal Victoria Military Hospital in Netley, on England’s south coast.
Lieutenant Graves
Graves had gone straight from Gallipoli “into line & through Somme.” In fighting around Beaumont Hamel in France, a shell had landed “quite close & blew him up.” Dazed, he was helped to the company dugout, after which he “Managed to carry on for some days,” although an ominous “Weakness of R[ight] side was developing steadily.” Ironically, it was precisely the soldier’s ability “to carry on” that had aroused skepticism over the real nature of his malady.
Suicide Rates During and After WWI
The worst figures regarding WW I suicide rates happened in the years following the Great War. The causes were due to what we now know as “P.T.S.D.” Unfortunately, the suicide of combat veterans years after their service is still all too common today. One can only imagine how bad it was in W.W.I. Combat trauma had various labels then. It was known as “Shell Shock,” “Combat Stress,” or “War Neurosis.” Combatants diagnosed as such were typically labeled “cowards” or believed to be “lacking in moral fiber.”
The “lucky” were discharged and sent home untreated. Authorities hospitalized a minority of the “cowards.” The military made examples of the “unlucky” soldiers and gave them a “field court-martial.” The trial resembled more of a “Mock trial” or “Kangaroo court.” They were found guilty, sentenced to death, and shot by their comrades. “Knowing they would face such action, and the disgrace associated with such issues, suicide amongst front line soldiers soared.”
Canadian Suicides
Jonathan Scotland, writing about the suicide rate in Canada during the First World War, has noted, “Not a single study exists on Canadian suicide in the First World War.” However, Scotland does mention a few Canadian soldiers who served during that war.
On 20 January 1919 Charles Campbell killed himself. The resident of Brockville, Ontario was the first of many veterans of the First World War to commit suicide that year. Others included Ross Puttilo, Alexander Fowler, William Bailey, and William Dowier. There would be more. Their deaths remind us that recent suicides in the Canadian military are part of a longer historical trajectory of soldier suicide.
Scotland listed male suicides by Age/Military Service in the Toronto Globe and the Toronto Daily Star newspapers one year after reporting the Armistice signed in 1919. The Toronto Globe revealed that42 the total number of male civilian suicides was 57%, compared to 43% of the veteran population. From 1880 to 1900, all male suicides comprised 28% civilian and 72% veteran. The Daily Star, covering the exact statistics, found 69% civilian suicides to 31% veteran. From 1880 to 1900, 20% were civilians compared to 80% veteran suicide rates. This rate means that in 1919, about 40% of all reported suicides in Toronto, Canada were on the veteran side.
Moreover, if only the suicides of men aged 18-39 (those most likely to serve) are considered, then the percentage of reported veteran suicides doubles to nearly 80%. Clearly the suicides being reported in the press were disproportionately soldier suicides.
Economic difficulties encountered by Capt. William Dowler of the Canadian Medical Corps led to his suicide in November 1919. He refused, due to his pride, any financial aid. Often, the men mentioned above, and those not described, became “despondent.” Some had suffered tremendous wounds; others had not. Employment varied as well. “But one thing is clear: their suicides are invariably attributed to the war. Moreover, in The Globe and The Star, the reports show no sign of shock, shame, or surprise at this conclusion. Indeed, in almost every case, the war is widely accepted and unchallenged as the cause of their suicide.”
New Zealand and Australia
Compared to “Australia, Great Britain, and the United States—in wars since World War I,” the New Zealand soldiers “suicide rate is nearly twice as high as American World War I soldiers treated in V.A. hospitals in the 1920s, but identical to that observed by Minogue in his study of World War I veteran suicides in New South Wales.”
In New Zealand, statistics revealed that suicides among returning veterans from the Great War ranged from two to four times as high as men not having gone to the front. Queensland, Australia’s statistics are quite similar to those of Canada, post-war.
One unnamed blogger has written a dissertation about suicide in WWI. His purpose was phrased with a question mark, “Suicides in World War One?” He noted, for instance,
Unfortunately, suicide was quite widespread due to varying factors. It was especially a problem on front line areas where the worst horrors of WW I were known to occur. The more frequent cases were invariably on the British and French front lines, where soldiers in general could expect to remain on the front line for longer periods than their counterparts in the U.S. Army for example (after their entry), or even their enemy in the German trenches.
Desertion was an increasing problem from those suffering conditions such as “shell shock,” the usual penalty, a firing squad. Companies of French soldiers “mutinied" at points of the worst fighting, however, few were punished for doing so, unlike the British.
Whilst there are very few statistics on how many suicides there were exactly, soldiers suicided by varying means, usually their own weapon or grenade. Others simply went over the top of the trench they occupied knowing full well they’d be shot by the enemy, a phenomenon we know today as “Suicide by Proxy,” but nevertheless an act of suicide.
Britain
The Journal, a British newspaper, printed the May 28, 1915 headlines and article as follows,
SOLDIER AND HIS WIFE ASPHYXIATED.
REMARKABLE EVIDENCE AT THE INQUEST.
DID NOT WANT TO BE PARTED.
Under two pictures of the deceased printed in the Journal were published these final words,
Shadrach Critchley, 35, and his wife Annie, 45, were found lying side by side on a mattress at their home in Leigh, Greater Manchester, on Monday May 24 1915 - shortly after Mr Critchley was recruited to the army.
According to friend and fellow soldier Richard Adamson, he was at the Fleece Inn the night be-fore he was due to rejoin his regiment, telling him he had made a mistake in enlisting in the forces.
Mr Adamson said he had tried to reassure him it would be fine but when he went to the Critchleys’ house the following evening, he forced open the door and found both Shadrach and Annie on a mattress on the kitchen
floor.
An inquest heard the couple had written notes expressing their wish not to be parted, and were buried together in St Paul’s churchyard in Westleigh. At the inquest, the jury, who heard evidence concerning their deaths, recorded a verdict of temporary insanity.
Mr Critchley’s name was finally given posthumous recognition when he was placed on the Brookwood Memorial, in a list of around 500 men who died on British shores.
Gallipoli
Future British Major Guy Nightingale would survive the horrors of the Gallipoli campaign without a scratch. After the Gallipoli disaster, the British military transferred its unit to the Western Front in France. He left the service in 1926, and retired to Somerset but struggled to adjust to civilian life. He died by suicide in April 1935, the 30th anniversary of his landing at Gallipoli, having suffered from alcoholism and depression.
On April 18th, 1935, in the peaceful English village of Wedmore, in Somerset, at the quaint address of Thatch Cottage, Guy Nightingale died within a week of the 20th anniversary of his landing on V Beach. Three causes of death were listed on his death certificate: cardiac syncope, delirium tremens and chronic alcoholism. Some said Nightingale died by his own hand; a doctor now might simply at-tribute the ending of his life to post-traumatic stress disorder.
Irish Suicides
Since Ireland fought alongside British soldiers, we would expect suicide rates to be comparable for both British and Irish soldiers. What was discovered is quite interesting. “(D)using the 5 years of the First World War, there was a significant reduction in suicide rates for men by 18.9% (95% CI 3.7 to 24.2).” Male suicides declined. After the conclusion of hostilities, French suicides declined, although there was the potential for under-reporting deaths by suicide by local registrars. Émile “Durkheim’s so- cial theory of suicide indicated that Irish men may have focused on the collective goal of defending their island rather than their suicidal wishes during the 1914–1918 war.”
French Suicides
Painkillers, including aspirin which “they consumed in astonishing amounts,” according to Sliosberg, were heavily prescribed: pyrethane, nealgyl, sedatives, or vitamin B1 coupled with physiotherapy, radiotherapy or ionization. “These methods fail or even aggravate the situation,” explained the same author. The surgeon Leriche highlighted the use of morphine and its consequences: severe constipation (lasting eight to ten days) and addiction or dependence, with the alternative being sometimes suicide. Leriche wrote: “We must not let them become morphinomen: the amputee with an addiction to morphine is incurable. Sooner or later, he will reoffend. Believe me, I cared for forty of them.”
The war created new societies in France. The disfigured formed groups of men whose faces had been mutilated beyond recognition, known as the association “the broken faces” and l’Union des Blessés de la Face. This horror drove many disfigured men to suicide, although this self-inflicted death was rare. The doctors and staff didn’t mention suicides, but they knew it occurred.
Amputees gathered in their companies for support. Pain, unknown before the war, was their constant
companion. “(T)he wounded now belonged to a group of stigmatized men, their faces ravaged by war, seemingly inhuman.”
British Suicides
In 1916, a young British private in northern France wrote home to his parents explaining his decision. to take his own life. A survivor of the early days of the Somme, considered one of the most brutal battles of World War I, Robert Andrew Purvis apologised to his family before praising his commanding officers and offering the remainder of his possessions to his comrades. Purvis’s surviving suicide note remains one of the only documents of its kind from World War I.
The Most Famous American Suicide of the First World War
Col. Charles Whittlesey
Few of us today know the story of Col. Charles Whittlesey and the Lost Battalion. Their heroics are the stuff of legend. The Great War Society has compiled the following:
In Europe, Whittlesey served with the 77th Division, 308th Battalion, Headquarters Company. He was involved in defensive endeavors, first behind the British front and later in the Luneville Defensive Sector. Beginning in August 1918, Whittlesey’s Division entered real combat in the Vesle, Aisne, Argonne and Meuse offensives. Whittlesey gained world-wide recognition in October 1918 when the companies of his battalion, which were part of a campaign against the Germans in the Argonne Forest, were cut off for several days without adequate supplies of food or ammunition. Though it was often blamed on Whittlesey’s own overzealousness and inexperience, the troops of the 308th were left vulnerable to being surrounded by the enemy. Their own successful advance, and the inability of the Allied troops on the flanks of Whittlesey’s advance, had left them in such a position.
On October 2nd, when the companies of Whittlesey’s battalion and other units assigned to the 308th Infantry were first surrounded, they numbered 463 men. Parts of other units including some men of the 307th Infantry under the command of Nelson Holderman joined the main group bringing the total trapped to about 550. By October 7th, when Whittlesey’s troops were rescued, they had been reduced to 194, alive and unwounded. While the 308th Infantry was cut off in the “Pocket,” a hill between Charleveaux Brook and the old Roman road and railroad in that sector, they were subjected constantly to machine gun and trench mortar attacks by well-supplied German troops. In addition, the trapped men suffered from what is now called “friendly fire.” The runner chain from the ‘Pocket’ to Headquarters had been broken and the only means of communication was by use of homing pigeons. Unfortunately, one of the pigeons brought somewhat inaccurate coordinates back to headquarters. After much additional suffering, the last pigeon, Cher Ami, was used on October 4th to stop this friendly barrage. . . .
Early on October 7th, before the relieving Allied troops arrived, the German Commanding Officer who surrounded the Americans sent a letter to Whittlesey by an American prisoner requesting his battalion’s surrender. Whittlesey and George McMurtry, his second-in-command, refused to acknowledge this request and even pulled in the white panels used to signal Allied planes for fear the Germans would mistake them for surrender flags. It was widely reported in the American press that Whittlesey had responded “Go to Hell!” immediately upon reading the letter. He later denied having made the statement, suggesting that no reply was necessary.
The eventual relief occurred when several runners were able to break through the German lines to the south and lead the advancing troops to the ‘Pocket.’ Whittlesey was promoted from Major to Lieutenant Colonel upon the relief of his beleaguered troops. He was relieved from further duty on October 29th and returned to the United States. On December 5th, through the issue of Special Order No. 259 from Headquarters at Fort Dix, NJ, he was honorably discharged from the United States Army. The following day, December 6th, he was named a recipient of the Medal of Honor, the highest award given by the U.S. Army. His subordinates, Capts. McMurtry and Holderman would also be awarded Medals of Honor for their service in the pocket. . . .”
Congressional Medal of Honor Society reported the following:
On November 11, 1921, Whittlesey participated in the burial of the first Unknown Soldier and two weeks later he boarded the British steamship SS Toloa bound for Havana, Cuba. According to the Captain of the Toloa, on the evening of November 26, Whittlesey dined at the Captain’s Table and
appeared in good health and spirits and entered into a lively discussion on football, manifesting an active interest in the Army and Navy football game being played that day…. After dinner he repaired to the smoking salon … and talked with [Mr. Wilmot] for more than two hours on a wide range of subjects. [He,] Mr. Wilmot noted nothing unusual … (Langbart, 2018).
Whittlesey returned to his stateroom shortly before midnight and was never seen again.
World War II (1939-1945)
World War II was the most destructive conflict in history. It cost more money, damaged more property, killed more people, and caused more far-reaching changes than any other war in history. Godfrey Dodson, Gadi Farfour, and Allison Sturgeon discovered the following facts,
D Day Landings. Omaha Beach, June 6, 1945.
Of the 800,000 American soldiers who fought the Germans in WWII, 37.5% were diagnosed as severe psychiatric cases and thus discharged. Five hundred four thousand Army veterans “were lost to the fight for psychiatric reasons. Another 1,393,000 suffered symptoms serious enough to debilitate them for some period.”
As the events of World War II unfolded, psycho-analytic concepts underwent modifications, and multiple analytic concepts were used to interpret war-related neurosis. These theoretical concepts represented an attempt to explain the multiple symptoms seen in war neurosis in terms of an intrapsychic model, which downplayed the role of the trauma itself.
Psychiatric studies conducted in Canada, America, and Britain during the Great War observed in their soldiers: “acute exhaustion, war fatigue, war neurosis, and old soldier’s syndrome.” In 1945, Saul formulated combat fatigue and fight or flight, which became common parlance in psychology.
Lt. Col. Dave Grossman has described twentieth-century warfare, stating, “In every war in which American soldiers have fought in this century, the chances of becoming a psychiatric casualty—of being debilitated for some time as a consequence of the stresses of military life—were greater than the chances of being killed by enemy fire.”
Eugene Sledge, author of With the Old Breed: At Peleliu and Okinawa, wrote, “The Japanese fought to win—it was a savage, brutal, inhumane, exhausting and dirty business. Our commanders knew that if46 we were to win and survive, we must be trained realistically for it whether we liked it or not. In the post-war years, the U.S. Marine Corps came in for a great deal of undeserved criticism, in my opinion, from well-meaning persons who did not comprehend the magnitude of stress and horror that combat can create. The technology that developed the rifle barrel, the machine gun and high explosive shells has turned war into prolonged, subhuman slaughter. Men must be trained realistically if they are to survive it without breaking, mentally and physically.”
Iwo Jima. 23 February 1945. U. S. Marines of the 28th Regiment, Fifth Division, hoist an American flag atop Mt. Suribatchi, Iwo Jima volcano, after battling the Japanese to the top of the crater. Platoon Sgt. Earnest Ivy Thomas, aged 21 of Tallahassee, Fla. was the Marine who raised the flag, during the height of the Suribachi battle Friday. Thomas broke out the three-foot-long ensign while his company was under sniper fire. The small flag as supplanted soon by a larger one on a high staff which all members of the group helped to carry to Suribachi's 566-foot crest. Photo by Associated Press Photographer Joe Rosenthal on assignment with the wartime still picture pool.
While I attended the combat trauma groups at Jefferson Barracks, MO, post 9/11, the film Saving Private Ryan came out. A Psychiatrist working in the mental health section told me that many WWII veterans had started showing up at the emergency ward and then transferred to the mental trauma unit at Jefferson Barracks. They swamped the ward, which confirms Dr. Michael Robertson’s findings: “We’re. . . seeing a large number of older veterans. Quite a lot of them are presenting with nightmares, intrusive memories of the war which are quite disabling for them.” Many had shown no signs of the disorder until much later in life. They had no history of mental illness. Nightmares are symptoms demonstrated by people who have experienced automobile accidents, whereas, in aging Vietnam veterans, there is “more irritability, avoidant behaviour.” The onset of symptoms of combat stress has resulted from the bias of film or print media against suffering veterans. Unfortunately, researchers and scientists are unsure why some older veterans succumb to traumatic stress.
A 2016 study stated, “The generalization of fear is an adaptive, behavioral, and physiological response to the likelihood of threat in the environment. In contrast, the overgeneralization of fear, a cardinal feature of posttraumatic stress disorder (P.T.S.D.), manifests as inappropriate, uncontrollable expression of fear in neutral and safe environments. Overgeneralization of fear stems from impaired discrimination of safe from aversive environments or discernment of unlikely threats from those that are highly probable. In addition, the time-dependent erosion of episodic details of traumatic memories might contribute to their generalization.” (emphasis added)
The study added, “The efficient processing of threatening and fearful stimuli is central to generation of adaptive behavioral and physiological responses. Inability to disambiguate safe from threatening stimuli or to calibrate physiological responses to uncertainty of threats can produce uncontrollable expression of fear, dysregulation of stress hormones, and sustained anxiety states. Exposure to traumatic events or stressful life experiences is known to tax our fear and threat processing systems. It is therefore not surprising that although the lifetime prevalence of generalized anxiety disorder (G.A.D.) and posttraumatic stress disorder (P.T.S.D.) is between 5 and 10% in the general population, the prevalence of P.T.S.D. is of greater magnitude in individuals repeatedly exposed to trauma (20–30%)” (emphasis added)
Alexander McFarlane discovered that the ongoing stress of combat strained both mind and body, resulting in hypertension and chronic pain.
There is longstanding interest in the effects of stress on health, due to the strain that it places on the adaptive capacity of individuals, which thereby leads to an increased risk of disease.
The effects of stress on the hypothalamic pituitary adrenal axis (HPA) and the autonomic nervous system have long been studied and the regulation of these systems has been referred to as “allostatic load.” This refers to the wear and tear on the body in response to repeated cycles of stress. This phenomenon has the potential to be manifest in various ways, influenced by the interaction with other personal and environmental risk factors for disease. Hence, the physiological dysregulation that underpins allostasis represents a final common pathway to disease that can be manifest in various ways.
Today, one method of treating people with a mental health condition is known as “COSR” or Combat and Operational Stress Reaction diagnosis. Doctors expected complete recovery within 72 hours. As we have seen, the acronym “PIE” was adopted during WWII, which stood for “proximity, immediacy, and expectancy.” Delays in treatment could undermine the healing process. A soldier could return to his unit if, after rehab, the medical personnel believed him had recovered.
Suicide Rates During and After WWII
In California, reports have surfaced that some of the “Greatest Generation” have decided to conclude their lives by suicide. This is “roughly double the rate of veterans under 35, those who are returning home from Iraq and Afghanistan,” Aaron Glantz wrote four years ago. Glantz discovered that 532 veterans living in California, all over 80 years old, had killed themselves between 2005 and 2008. Glantz interviewed 86-year-old Ken Norwood for his piece. Norwood was shot down over Belgium while on a bombing raid in a B-24. He awoke in a German field hospital because the impact of the crash threw him out of the bomber. That began his cattle car adventure across Europe at the behest of the Third Reich. He says that he was kept underground and alone in a cell. His toilet was a trench. Mr. Glantz said he’s gotten used to the flashbacks that play in his head like a DVD. As he ages, however, the flashbacks have gotten worse. “I have fewer activities in daily life now. I don’t have a professional career to pursue or a family to come home to,” he stated. “My kids are grown. They have their own lives.”
Kerri Childress, the U.S. Department of Veterans Affairs spokeswoman, conceptualizes the high incidence of suicide among World War II veterans. In this statement, she writes, “We didn’t even recognize mental health as an issue when they returned,” she said. “Nobody was recognizing it and nobody was talking about it, and it was certainly not something that they could get care for from the VA.”
After the Revolutionary War, the War of 1812, the Civil War, and World War I, one would think that PTSD was going to surface at some point in the Second World War. It appears not. Psychological trauma, therefore, was not factored into pre-war planning. Only once the cases began to reveal themselves, wholesale did the realization that regardless of which conflict, men have a point of mental stress they are incapable of moving past. Most, if not all, of the research on neurosis began after the war started, with most of it collected and studied post-war.
Treatment
In World War II, authorities attempted to avoid the horrific casualty levels seen in World War I. They administered psychological screening tests to eliminate those who could not tolerate battle. It was concluded that the tests were a failure, and there were very few rejected recruits. Soldiers who suffered from shell shock in World War II needed continual “forward treatment.”
The History of P.T.S.D.: The Korean War to Afghanistan
The Korean War (1950-1953)
The war fought in Korea is today commonly called “The Forgotten War.” Far too many people today are uninformed about this costly conflict. President Harry S. Truman declared the war a “police action” because he never asked Congress to pass an official war declaration. To the men on the ground and those flying close air cover, it was nothing less than a kill or be killed, a real shootin’ war. Twenty countries fought in the Korean War, and three of the twenty countries fought as aggressor nations: North Korea, Russia, and China, although the Russians denied any involvement until 1989. Nearly 5 million people died. More than half of these–about 10 percent of Korea’s prewar population–were civilians.
First Lieutenant Baldomero Lopez, USMC, leads the 3rd Platoon, Company A, 1st Battalion, 5th Marines over the seawall on the northern side of Red Beach, as the second assault wave lands, 15 September 1950, during the Inchon invasion. Wooden scaling ladders are in use to facilitate disembarkation from the LCVP that brought these men to the shore. Lt. Lopez was killed in action within a few minutes, while assaulting a North Korean bunker. Note M-1 Carbine carried by Lt. Lopez, M-1 Rifles of other Marines and details of the Marines' field gear.
By 1949, Mongolia, China, and North Korea, spurred on by Russia and China, reached a boiling point. The Communist North Koreans moved south, conquering the South Korean army and a few American units. The Communists captured South Korea’s capital, Seoul. They kept driving the Americans and South Koreans south to Pusan, where America and South Koreans formed a pocket around that city, buying time for the U.S. to send in reinforcements and supplies to push the aggressors back north.
My father was a Navy flight instructor during WWII because he didn’t receive orders for a fighting unit, and that “oversight” by the Department of Defense disappointed him. Instead, he instructed Navy cadets in flight training. By the time Dad’s enlistment ended, the North Koreans invaded their neighbors to the south, intent on unifying the country under Communism. Dad and some of his buddies carried their Navy discharge papers and walked down the hall to join the Marine Corps Reserve. These men wanted to fight. For reasons not completely clear to me, Dad began flying helicopters. After flight training, he and many other men learned to fly repeatedly in rotary wing. With their orders, these men were assigned to Marine Aircraft Group (MAG) 33.
I only heard one anecdote about my father’s war experiences while growing up. During one medivac mission in the Korean mountains, Dad said the clouds covered the massifs, which forced him to fly on instruments. He couldn’t use his map, so he descended in search of landmarks to find his way. During this nail-biting time, he saw a road and followed it to reach the wounded Marines. Flying mere feet off the deck toward his destination, he found himself almost eyeball to eyeball with an American military truck driver coming straight at him. To say they both were simultaneously surprised and scared would be an understatement.
Besides that event, I knew little about Dad’s tour in Korea. It was not until his funeral in January 2001 that I learned of an event that undoubtedly had a negative mental effect on him, as well as our family and me personally.
A Marine unit called for a medivac. One of the grunts somehow got his leg or foot stuck when crossing a river near the ocean. The tide started coming in, so the Marine needed immediate extraction. Dad found the Marine’s location, and while hovering over the Corpsman working on him, it became clear that with the rising water, the Marine would need to have his leg amputated, so he flew back to the ship to find a doctor. Upon return, the doctor removed the man’s leg in time to save him from drowning.
On another occasion, my father was awarded the DFC (Distinguished Flying Cross) for heroism in rescuing several more wounded Marines during a particularly stormy night. His S-19 Sikorsky did not come with night navigational aids, which made the mission all that more heroic. He rescued those men and received a medal for it. Very few men could match my father in the air.
Marines fought back fifteen miles through Chinese hordes, where they organized for the epic 40-mile fight down mountain trails to the sea.
The British Journal of Psychiatry surveyed Australian Korean War veterans fifty years after the war. Some of their findings are as follows:
Within the veteran’s group, increasing odds of meeting criteria for P.T.S.D. or depression were both associated with increasing combat exposure, decreasing level of rank, increasing the duration of deployment, being first deployed before the armistice, and being wounded in action. There was also an association between both psychological health outcomes and Service branch, with Army veterans demonstrating the greatest odds of P.T.S.D. or depression, followed by Navy veterans, and with Air Force veterans demonstrating the lowest odds. The association between P.T.S.D. and increasing level of reported combat exposure was particularly strong, with veterans who reported heavy combat almost 15 times more likely to meet criteria for P.T.S.D. than veterans who reported no combat. The dose-response slope indicates that the expected increase in the odds of P.T.S.D. per categorical increase in combat exposure level (e.g., from moderate to moderate-heavy) is 65%. The association between depression and combat exposure was also strong, with a 37% expected increase in the odds of depression per categorical increase in combat exposure level.
The other most notable association was with rank; with enlisted ranks being four times more likely – and non-commissioned officers three times more likely – than officers to meet criteria for P.T.S.D. Enlisted ranks and non-commissioned officers were also more than twice as likely as officers to meet the criteria for depression. The dose-response slopes indicate a 54% increase in the odds of P.T.S.D. and a 43% increase in the odds of depression per categorical decrease in rank.
The likelihood of P.T.S.D. was doubled in veterans who reported being wounded in action (regardless of evacuation type) compared with veterans who did not report being wounded and almost halved in veterans who were first deployed to Korea after the armistice compared with veterans who were first deployed during the earlier phases of the war. Similar patterns were observed for depression, but the associations were not so strong. Increased deployment duration was associated with an expected 27% increase in the odds of P.T.S.D. and a 10% increase in the odds of depression. Furthermore, P.T.S.D. – but not depression – was associated with being younger and having fewer years of service experience when deployed. Additional analysis (not tabulated) indicated that Korean War veterans who had been deployed to other major conflicts did not have worse psychological health than veterans who had not been deployed to other conflicts.
The study results suggest a complex interrelationship between characteristics of war service and subsequent long-term psychological ill-health. Combat severity and duration, war related injury, inexperience, lack of seniority, and youthfulness all contribute to long-term psychological morbidity.
Treatment
Medical professionals discontinued the forward treatment of psychological cases and removed them from the front lines. Instead, “rest and relaxation” (R & R) replaced forward treatment. The general medical consensus was a frequent rotation of troops. However, Colonel Albert J. Glass fought to have the hard-won principles of “forward treatment” reimplemented in previous wars. The newest approaches to psychological treatment discovered that approximately 90% of the troops suffering psychological distress resulted after returning to the front lines.
On the Korean War Educator website, researcher Jim Goodwin stated, “During the Korean War, the approach to combat stress became even more pragmatic. Due to Albert Glass’s work, each breakdown found doctors treating patients in a situational manner. Clinicians once again provided immediate onsite treatment to affected individuals, always expecting that the combatant would return to duty as soon as possible. The results were gratifying. During World War II, 23 percent of the evacuations were for psychiatric reasons. But in Korea, psychiatric evacuations dropped to only six percent. It finally became clear that the combatant’s situational stresses were the primary factors leading to psychological casualty.”
During the Korean war, the APA Committee on Nomenclature and Statistics published the first Diagnostic and Statistical Manual of Mental Disorders (DSM). After World War II, military psychiatrists interpreted and then described “combat stress” characteristics. By defining the ‘reactions’ portion of “gross stress reactions,” these psychiatrists sparked the future road for proper treatment for veterans and civilians.
Suicide Rates During and After the Korean War
One study compared suicidality, an index derived from the severity of suicide attempts, between 320 World War II veterans, 199 Korean War veterans, and 4,619 Vietnam War veterans seeking treatment at VA facilities (Fontana & Rosenheck, 1994). Although more suicidality was observed in Korean veterans compared to Vietnam veterans, the difference did not reach statistical significance, and veterans from both of these wars were more suicidal than WW II veterans.
The Vietnam War (1964-1975)
The Journal of Psychiatric and Mental Health Nursing provides this observation: “Perhaps one of the most striking features of this case is that it concerns a very ordinary man living in a very ordinary street in a very ordinary catchment area. This does beg the question of how many other veterans of armed conflict suffer in silence from P.T.S.D. symptoms.” The next U. S. war, Vietnam, was a post-Korean War. Once again, the Vietnam Veterans had to fight the V.A. to have combat trauma recognized as a symptom of combat.
Combat operations at Ia Drang Valley, Vietnam, November 1965. Major Bruce P. Crandall's UH-1D helicopter climbs skyward after discharging a load of infantrymen on a search-and-destroy mission.
The term Post Vietnam Syndrome was used to describe returning soldiers with trauma symptoms. This syndrome usually consists of combat-related nightmares, anxiety, anger, depression, alcohol and/ or drug dependence, and poor responsiveness. The term post-traumatic stress disorder was not used in the DSM until the DSM-III was published in 1980 under anxiety disorders. Before that, this condition was viewed as stress response syndrome, which was a type of gross stress reaction. The policy for receiving treatment and compensation for P.T.S.D. for soldiers in the military during the war was that if the soldier experienced symptoms 6 months after their return home it was considered a “transient situational disorder.” This meant that it was a pre-existing condition that was not eligible for treatment by the United States Government. Even though the soldiers who were victims of P.T.S.D. did not receive compensation from the government, P.T.S.D. as a clinical diagnosis was evolving into a more complex and real disorder. This policy is unsettling to hear because P.T.S.D. can occur anytime after returning home from war, and many cases occur with delayed onset. This is referred to as chronic rather than acute, which is immediate.
The organization, Military Order of the Purple Heart, had stated, “By the time of the war in Vietnam, battle fatigue and shell shock had a new name - Post Traumatic Stress Disorder, or P.T.S.D. For over 40 years now, P.T.S.D. has been a signature problem for many Vietnam veterans and is one of the main conditions treated by the V.A. healthcare system today. It’s said to be197 one of the major causes of divorce for Vietnam veterans and, if some of the suicide statistics are true, P.T.S.D. is a major cause of suicide among Vietnam veterans.”
A study funded by the Department of Veterans Affairs estimated that more than 283,000 Vietnam veterans - men and women now beyond the age of retirement - still suffer post-traumatic stress disorder from their war experiences in Southeast Asia. One of the study’s key findings is that for some, P.T.S.D. is not going away since “it is chronic and prolonged. And for veterans with P.T.S.D., the war is not over.” These statistics may be too low. Although many Vietnam veterans may have experienced the symptoms of P.T.S.D., they were reluctant to report their illness, especially those who remained on active duty, for fear of being discharged under less than honorable conditions or being labeled as mentally ill. Others accepted a discharge under general or even dishonorable conditions to escape the harassment or embarrassing treatment. The Yale Law Clinic estimates that “as many as 80,000 Vietnam veterans were discharged with other-than-honorable status as a result of undiagnosed P.T.S.D., and less than two percent of those who have applied for discharge upgrades have been successful.”
U.S. Marines with Company G, 2nd Battalion, 7th Marines, direct a concentration of fire at the enemy during Operation Allen Brook, 8 May 1968.
The Disabled American Veterans organization set about assisting many veterans who received “bad-paper” discharges but who may also have struggled with PTSD. Unfortunately, these men separated from the military with undiagnosed symptoms of combat stress. During the Vietnam War, their “unacceptable” behavior became a cause for “O.T.H.” discharge or other than honorable dismissal.
In today’s military, P.T.S.D. is considered a mitigating factor for misconduct and behavioral problems. The military services are required to grant a medical evaluation to any service member who claims P.T.S.D. before finalizing a bad discharge.
The Pentagon's new rule comes in response to a federal lawsuit filed on behalf of several veterans in March that claimed the Defense Department was wrongfully denying discharge upgrade applications from veterans with claims and evidence of P.T.S.D. The new policy was applauded by the Yale Law School Veterans’ Legal Service Clinic, which is spearheading the federal lawsuit.
“DoD appears to be taking a significant step to correcting a longstanding injustice,” said Jennifer McTiernan, a student intern involved with the lawsuit. However, she said, it’s too early to tell how the new rule will be implemented and the lawsuit is likely to continue.
For years, the military services have rejected P.T.S.D. claims from Vietnam-era vets with what McTiernan called ‘Catch-22-like denials’ that say changes cannot be granted without a diagnosis of P.T.S.D. from the 1970s—even though P.T.S.D. did not become officially recognized by the medical profession until 1980.
Military planners understood to some degree that the conflict in Vietnam would produce many psychological casualties, and men exposed to the most significant combat had the highest rates of breakdown. In WWII and Korea, military leadership created a “points system” so that a soldier who accumulated a certain number of points left the field regardless of the war’s progress. The Department of the Army began a 12-month tour of duty before a soldier’s DEROS (date of expected return from overseas). The Marine Corps instituted a 13-month combat tour, or as we called it, “twelve and twenty” (twelve months and twenty days in the bush) before our tour ended, and we rotated home. The military planners also believed such action would prevent a sense of hopelessness that a soldier’s tour would never end, and thus a soldier or Marine did not have to hope to be wounded or killed to leave combat. His goal then became holding on for twelve months and twenty days, and he would board that freedom bird home to “the land of the round-eyes.”
Surprisingly, with American involvement in the Vietnam War, psychological battlefield casualties evolved in a new direction. What was expected from past war experiences--and what was prepared for--did not materialize. Battlefield’s psychological breakdown was at an all-time low, 12 per one thousand. It was decided that the use of preventative measures learned in Korea and some added situational manipulation . . . had solved the age-old problem of a psychological breakdown in combat. As the war continued for some years, some interesting additional trends were noted.
Although the behavior of some combatants in Vietnam undermined fighting efficiency, the symptoms presented rarely resembled the previous classical picture of combat fatigue. As the war progressed, a previously obscure but very well-documented phenomenon of World War II began to be re-observed. After the end of World War II, some men suffering from acute combat reaction, as well as some of their peers with no such symptoms at war’s end, began to complain of common symptoms. These included intense anxiety, battle dreams, depression, explosive aggressive behavior, and problems with interpersonal relationships, to name a few. These were found in a five-year follow-up and a 20-year follow-up.
The reported volume of neuropsychological incidents made Vietnam more problematic for U.S. combatants. During WWII and also in Korea, as the war dragged on, the cases of P.T.S.D. increased. At the wars’ conclusions, however, the number of cases decreased until it reached pre- war incidence. This decrease was not the case in Vietnam. Despite the prolonged nature of Vietnam and its intense fighting, neuropsychological patients did not increase until early 1970, at the height of Vietnamization. At that point, psychological cases increased dramatically. One website suggests that for many Americans, they
. . . were experiencing varying traumatic episodes other than combat. There were large numbers of plane crashes, natural disasters, fires, acts of terrorism on civilian populations, and other catastrophic events. The picture presented to many mental health professionals working with victims of these events, helping them adjust after traumatic experiences, was quite similar to the phenomenon of the troubled Vietnam veteran. The symptoms were almost identical. Finally, after much research by various veterans’ task forces and recommendations by those involved in the treatment of civilian post-trauma clients, the DSM III was published with a new category: post-traumatic stress disorder, acute, chronic, and/or delayed.
Suicide Rates During and After the Vietnam War
The United States lost over 58,000 American lives in the Vietnam War, which is still rising. One hundred thousand veterans or more have committed suicide post-DEROS/rotation. Over three hundred thousand U.S. personnel of the 2.5 million received Purple Hearts passing in and out of Vietnam. This number includes U.S.: 74,000 people with quadriplegia and multiple amputees. Four million Vietnamese were wounded, and that 1.5 million U.S. combatants suffer from P.T.S.D. due to the war. Suicides range to 100,000+. It is unknown how many Vietnamese, North or South, suffer from P.T.S.D. On any given night in America, roughly 150,000 veterans are homeless. Approximately 1 million boat people from Vietnam, Laos, and Cambodia became “boat people,” escaping the tyranny of the Communist North. Estimates are that half that many boat people perished on the open seas escaping Communism. Three million people became disabled “street people” in Vietnam after the war. Thirty-five thousand+ Vietnamese developed or were born with deformities from Agent Orange spraying. Fifty thousand+ Vietnamese, Laotians, and Cambodians died from unexploded ordinance left behind after the war while maiming sixty-seven thousand combatants. Finally, 400,000 Vietnamese were “re-educated” in 100 such camps post-war.
Alexander Paul contacted Point Man International, a Christian organization for veterans, to conduct a phone interview with a retired V.A. doctor. In that interview, the doctor estimated the number of Vietnam Veteran suicides at 200,000 men. The reason for the lower documented suicides primarily involved single-car drunk driving accidents and self-inflicted gunshot wounds but didn’t leave a suicide note or statement. According to the doctor, the under-reporting of suicides was primarily an act of kindness to the surviving relatives.
If the estimate of over 150,000 veterans of the Vietnam War has committed suicide since returning home is true, the figure would be almost three times the number killed in the war. When adding these deaths to the 50,000 plus Vietnam War dead, the number approaches the 292,000 American “combat deaths” of the Vietnam war.
The latest C.D.C. figures for the suicide rates in America from 1999 to 2010 discovered an increase of 28% of middle-aged U.S. citizens. Out of every 100,000 adults between ages 35 to 64 who committed suicide, it increased from 13.7 to 17.6 suicides. Many suicides arose from ages 50 to 54 (48%) and 55 to 59 (49%).
But suicide rates among Vietnam veterans are the highest of any particular group, according to John Draper, project director of the National Suicide Prevention Lifeline.
Treatment
The American Psychiatric Association released DSM-II in 1968 without listing the symptoms, signs, or definitions of “combat stress.” These omissions made it difficult to treat those returning home. Veterans began showing post-battle signs but without treatment. The doctors had no comparable evidence on which to base the symptoms and, therefore, no way to determine the best treatment. Without proper therapy, the Vietnam war veterans began self-medicating with drugs and alcohol.
It is also very important to note that throughout the history of this condition many soldiers exhibited no signs of P.T.S.D. until after their combat tours were over. They performed their duties admirably in combat suppressing the terrible things they saw and experienced in the war to get the job done. Only after the wars, upon reintegrating into society, the symptoms materialized and disrupted their lives. The “Post Traumatic” label is an important key to this, that means after the experience of war. Until recently, in the wake of Viet Nam, these veterans were largely forgotten and not treated by the V.A. mental health professionals who have a firmer grasp about how to teach vets to cope with P.T.S.D. Even today, more than half a century after their service, World War II veterans visit V.A. hospitals across the country to finally get help and relief from the psychological impairments they suffered from all these years. There should be no stigma attached to P.T.S.D., the average person couldn’t possibly fathom the stress, demoralization, and anger that being exposed to combat conditions can cause in an individual. War changes virtually every soldier permanently; there is no escaping that reality. Throughout the history of war, in all lands and all languages, it has been said about many veterans that they were never the same after coming home. That is the mark of P.T.S.D. Mental health professionals today have finally recognized that they must help and treat veterans who sacrificed so much to perform their role and service in combat and are deserving of the best medical help available.
My first awareness of the war’s effects on me came as I recuperated from malaria contracted on the night before leaving for R & R in Oahu, Hawaii, in 1968. Most Echo Co. Marines discarded the malaria pills the Corpsmen gave out because they often produced diarrhea. As I regained my strength, Tripler Army Medical Center’s malaria ward moved other patients and me to a large house 100 meters from the main hospital, which served as the final medical step before sending malaria-free patients back to Vietnam. However, it was not long before I started to hyperventilate and almost passed out. The doctors recognized this common symptom of psychological combat stress. They made an appointment for me to see a “certain doctor” on one of the Medical Center floors.
As I recall, that floor had only one exit for specific reasons, such as bringing in a new patient but not allowing him to leave at his leisure. I felt somewhat ill at ease as I entered and the door locked soundly behind me. I presented my medical records and waited for the doctor to appear. The doctor entered the hallway, and I gave him my records. Almost immediately, a patient wearing hospital pajamas, and whom I could tell was mentally ill, stepped up to the doctor. The patient saluted and then said something characteristic of the drill field at Boot Camp. This particular incident seemed out of place for a military hospital. It quickly dawned on me that I was standing in the psych ward, and that unnerved me. Now it made sense that my primary doctor had been evasive when he told him to report to this ward. He feared I might not make the appoint- ment if I knew my destination and the stigma that would surely accompany me back to my outfit.
The doctor and I sat down in his office, and he asked questions about my combat experiences. He wanted to know whether my return to combat troubled me? I told him I didn’t want to go back, but I had no choice. Regardless, it was my responsibility to return to my unit. The doctor seemed satisfied with my answers, and fifteen minutes later, he saw me at the door. My hyperventilating resulted from anxiety, and it was “cured” by placing a paper bag over my mouth into which I breathed my carbon dioxide.
Tripler Army Medical Center treated me with the utmost care and dignity during those long, painful days recuperating from malaria. The doctors and nurses took exceptional care of this Marine.
Gulf War (1991); Iraq and Afghanistan War (2002 to present)
U.S.A. Today reports that the Pentagon has officially listed 2,355 service personnel as killed in action in Iraq and Afghanistan since the start of those wars. Approximately 697,000 U.S. Veterans served in the Persian Gulf War, and more than 263,000 have since sought medical care at the Department of Veterans Affairs. Over 185,000 have filed claims with the Veterans Administration for service-related medical disabilities, including significant physical and psychological distress attributed to their participation in the operations.
SOUTHERN IRAQ -- Soldiers from the 3rd Infantry Division under the command and control of U.S. Army Europe's V Corps take up firing positions during an enemy approach on their position at objective RAMA, in southern Iraq, March 24, 2003. Operation Iraqi Freedom is the multinational coalition effort to liberate the Iraqi people, eliminate Iraq's weapons of mass destruction and end the regime of Saddam Hussein. (Photo by Sgt. Igor Paustovski)
The U.S. Department of Veterans Affairs estimates that P.T.S.D. afflicts:
• Almost 31 percent of Vietnam veterans
• As many as 10 percent of Gulf War (Desert Storm) veterans
• 11 percent of veterans of the war in Afghanistan
• 20 percent of Iraqi war veterans
What is most perplexing about the Gulf War is what has come to be known as Gulf War Syndrome due to U.S. participation there. Doctors and researchers have diagnosed three distinct symptom types:
• Fatigue.
• Mood and cognition problems (for example, feeling depressed, having difficulty remembering or concentrating, feeling moody, feeling anxious, having trouble finding words, having difficulty sleeping).
• Musculoskeletal problems (for example, joint pain, joint stiffness, and muscle pain). Within these categories, symptoms can vary in type and severity.
President George W. Bush appointed several committees to study these symptoms from the war to advise the U.S. Government on how to treat these veterans. Evidence suggests that certain conditions could cause and thus increase a veteran’s risk of developing this illness.
These risk factors include exposure to the following: extremes of heat and cold, blowing dust, smoke from oil-well fires, petroleum fuels and their combustion products, pyridostigmine bromide (administered as pretreatment for potential poison-gas exposure), anthrax and botulinum toxoid vaccines, depleted uranium (used in certain artillery shells), infectious diseases, chemical warfare agents (such as sarin gas), pesticides, and pervasive psychological and physiological stress. Researchers have explored different hypotheses to explain the physical and psychological reactions to toxic exposure, but current scientific research does not consistently support any single explanation.
The jury is still out as to the exact causes of the syndrome. Some researchers suggest that PTSD-like symptoms do not account for the Gulf War Syndrome range: Only toxic exposure must be responsible for this disorder. The President’s Advisory Committee on Gulf War Veteran’s Illness attributes to and is documented by “the psychological and physiological symptoms result from combat stress.” Scientists and researchers need to do more study.
SOUTHERN IRAQ -- Soldiers from the 3rd Infantry Division under the command and control of U.S. Army Europe's V Corps take up firing positions during an enemy approach on their position at objective RAMA, in southern Iraq, March 24, 2003. Operation Iraqi Freedom is the multinational coalition effort to liberate the Iraqi people, eliminate Iraq's weapons of mass destruction and end the regime of Saddam Hussein. (Photo by Sgt. Igor Paustovski)
Top Left: Marines in the middle of a sand storm make their way back to their vehicles after dismounting and patrolling a nearby mountain ridge in Bakwa, Farah province, Afghanistan, May 3. The Marines of Company I, 3rd Battalion, 8th Marine Regiment (Reinforced), the ground combat element of Special Purpose Marine Air Ground Task Force - Afghanistan, are operating in Bakwa to maintain security in the rural area. U.S. Marines are in Afghanistan to reinforce success and sustain the momentum of the ongoing progress by alliance forces. Company I's mission is to conduct counterinsurgency operations while training and mentoring the Afghan national police. Special Purpose Marine Air Ground Task Force.
Top Right: As seen from the cockpit of the lead aircraft, two F/A-18 “Hornet” strike fighters assigned to the "Wildcats" of Strike Fighter Squadron One Three One (VFA-131) conduct combat missions over Afghanistan. The "Wildcats" are part of Carrier Air Wing Seven (CVW-7) embarked on board USS John F. Kennedy (CV-67), currently deployed in the region in support of Operation Enduring Freedom. U.S. Navy photo (RELEASED)
Centre: Spc. Gareth Warner drops a 120mm mortar round into the tube while Spc. Ricky Olivo keeps the gun on target during a fire mission on Combat Outpost Zurok in Paktika province, Afghanistan, July 13. The Soldiers are deployed with the 3rd battalion, 509th Airborne Infantry Regiment, 4th Brigade Combat Team, 25th Infantry Division. (Photo by U.S. Army Staff Sergeant Andrew Smith, 55th Signal Company.)
Bottom Left: U.S. Army Pfc. Branden Hazuka, assigned to 2nd Battalion, 377th Parachute Field Artillery Regiment, 4th Brigade Combat Team, 25th Infantry Division, searches a qallat, or an Afghan home, for explosives and weapons during an air assault mission in Khost province, Afghanistan during Operation Champion Sword, Aug. 2. Afghan national security forces and International Security Assistance Forces teamed up for the joint operation, targeting specific militants in eastern Afghanistan.
Bottom Right: Marines with the Marine Expeditionary Brigade-Afghanistan prepare to board buses on May 3, shortly after arriving in southern Afghanistan.
Afghanistan Photo by Lance Cpl. Brian D. Jones.
The Iowa Persian Gulf Study Group discovered that 2% of Gulf War veterans suffered from PTSD. From 4% to 9% of Army veterans, after returning home, developed psychological symptoms within the first five days of arrival. The highest-risk veterans with P.T.S.D. were females because they already had a “pre-combat abuse history.” Subsequent studies revealed that rates of P.T.S.D. increased as time passed, 3% for men and 8% for women.
Approximately 22 percent of Iraq and Afghanistan war veterans who sought care at the Veterans Administration suffer from post-traumatic stress disorder and 17 percent from depression, researchers at the San Francisco V.A. Medical Center and the University of California-San Francisco reported in 2009.
A 2008 Rand Corporation study, based on a smaller sample than the V.A.-UCSF study but including veterans who did not enroll at V.A. health centers, found that 14 percent of Iraq and Afghanistan war veterans are affected by P.T.S.D. and 14 percent by major depression.
Stanford University and Naval Postgraduate School researchers who examined the delayed onset of P.T.S.D. found that, by 2023, the rate of P.T.S.D. among Iraq war veterans alone could rise as high as 35 percent.
“A new study conducted in the United States and published in the May 2007 issue of the British Journal of Psychiatry has found that deployment in the Gulf War has been associated with increased levels of mental disorders, psychological symptoms, and a lower quality of life, beginning during the war and persisting at a lower rate ten years later. The National Health Survey of Gulf War Era Veterans and Their Families included postal and telephone surveys conducted among 15,000 deployed veterans and 15,000 non-deployed veterans, beginning in 1995. Overall, the findings point to the need for adequate follow-up mental health care for veterans with persistent mental illnesses following major military deployments.”
“One in five veterans of the Iraq and Afghanistan wars are diagnosed with post-traumatic stress disorder (P.T.S.D.) – over 300,000 veterans by the end of 2012. The social and economic costs of P.T.S.D. are immense. First-year treatment alone costs the government $8,300 per person or more than $2 billion so far.”206
Jeremy Proffitt
Jeremy Proffitt struggles with his role in Iraq and Afghanistan. “I came home from Iraq in March 2004, yet I’m still fighting a war, a war here at home. It’s a war of shadows, one that no one seems to understand. A war of anger and anxiety fought in the recesses of my mind. Like in the two wars I fought in Iraq and Afghanistan, I don’t know who the enemy is. There, insurgents take potshots at you, then go back into hiding. Combating post-traumatic stress disorder, P.T.S.D., is the same. Some days I feel as if I have the enemy on the run; other days it has me pinned down.”
Rob Withrow
Reporter Carol Smith filed this report: In November 2003, he went to Iraq with the 1st Battalion, 35th Field Artillery Regiment. When he returned a year later, he received an Army Commendation Medal for “Exceptionally meritorious service as an air guard during Operation Iraqi Freedom.” His attorney confirmed he had no disciplinary record before returning from Iraq and consistently received good-conduct medals. A memorandum from his first sergeant with his old brigade noted, “I would gladly serve with S.P.C. Withrow in combat again because I believe him to be a true Warrior.”
“Tall and lean with trimmed dark hair, Withrow is personable and straightforward while relating his story. The bluish circles under his brown eyes betray fatigue. In addition to his legal and health problems, he faces bankruptcy and loss of his base housing. Rob worried about his wife and three children if he goes back to Iraq. “I don’t want them to wind up on the street,” he said. “When he got back, I could tell he was just different,” said Jenny Withrow, his wife of six years.
“First it was the horrors of Iraq. Now, Rob Withrow is locked in a fight with his own Army superiors. He wants mental health treatment — they want him to face a court-martial.” Rob Withrow was a good soldier until Rob returned from combat duty in Iraq. By his admission, Rob is no longer anyone’s idea of a model-fighting man. He screwed up, and he’s screwed up —an assessment with which the Army agreed. Since Withrow’s problems began, the Army reduced his rank from sergeant to private. But that’s where his and the Army’s agreement ends.
Withrow wants mental health treatment. He has tried to commit suicide four times since returning from Iraq. He has been hospitalized in Madigan Army Medical Center’s inpatient psychiatric unit on multiple occasions and is currently on a cocktail of antidepressants and psychoactive drugs. He is a month out of treatment for an addiction to narcotic pain pills that he began taking to “numb out” the month he returned from Iraq. Now he does not fit the Army’s new criteria for deployment.
Estimates of the number of soldiers who suffer from P.T.S.D. and mental problems vary, but most experts agree that the nature of the fighting in Iraq sets up soldiers for psychological trauma. According to Ritchie of the Surgeon General's Office, an estimated 15 to 17 percent of deployed soldiers experience P.T.S.D., and 23 percent experienced other behavioral health problems. Others put the numbers higher. According to a study published last month in the Archives of Internal Medicine, nearly one-third (31 percent) of 103,788 veterans who had served in Iraq and Afghanistan were diagnosed with mental health or psychological problems upon their return.
The Surgeon General’s Office indicated about 11 percent of soldiers who have returned receive mental health diagnoses. For Withrow, as his mental anguish grew, his problems with his commanders intensified. “If I were his commander, I’d be frustrated with him as well,” said Pewees, who has also worked as a prosecutor. At the end of March, Withrow was informed he would deploy this week with the 50th Brigade, 2nd Infantry Division back to Iraq. As part of pre-deployment screening, an Army psychiatrist specified his “symptoms are not stable” and indicated he should have “no access to weapons or ammunition, no exposure to combat situations, no exposure to casualties, and was not recommended for deployment.” The issue of whether to send him to Iraq for a court-martial is still pending.
To make matters worse, the Army wants to redeploy him to Iraq, where it plans to court-martial him. The charges stem from his not showing up on time or sometimes at all. Withrow’s case raises questions about how the Army handles soldiers with psychiatric illnesses. Specifically, those with P.T.S.D. and depression. The Army wants to know whether discipline or its threat interferes with treatment.
Since his return from Iraq in November 2004, Withrow has received multiple Article 15s — the Army’s form of non-judicial punishment — for disciplinary issues related to “patterns of minor misconduct.” If the Army discharged him for misconduct, he would lose benefits for his family, which is already facing a financial crisis related to his demotions. “I’m not going to candy-coat it,” Withrow said. “I’ll take responsibility for my part. I have purposefully not gone to work.”
At the time, medical records revealed he was struggling with depression, anxiety, and post-traumatic stress disorder. He repeatedly informed doctors that he was late or absent from work because he was having difficulty waking up, in part because of potent sedatives prescribed for sleep disturbances.
A combat medic
One unnamed combat medic of Iraq states, “I can’t sleep at night. I lost my job. I used to train medics for Special Forces . . . I have a recurring dream . . . I worked on a soldier once who had been shot in the face . . . but in the dream, I go to my aid bag . . . and I come back from my aid bag . . . and I’m not working on that soldier anymore. . . (a long painful pause), but it’s my son . . . and every time he asks me why I can’t help him . . . that dream kicks my a$#.”
Every war has its after-war: depression, anxiety, nightmares, memory problems, personality changes, suicidal thoughts. If the studies prove correct, the wars in Iraq and Afghanistan have created roughly five hundred thousand mentally wounded American veterans.
Nic DeNinno, a veteran has had trouble adjusting to life at home after his combat tour. In “November, 2010,” . . . Nic “was in a twenty-three-bed psychiatric facility called Haven Behavioral War Heroes Hospital, in Pueblo, Colorado.” After counseling and anti-anxiety and antidepressant medications, “he was found one night in mid-flashback, driving in the wrong direction on a one-way street, the decision was made to send him to a residential treatment program for twenty-eight days. Twenty-eight days to get it fixed, as one of Nic’s sergeants said.”
He wrote about an early mission in Iraq:
“I don’t remember the exact briefing before we left but we were to show extreme force and to let these people know we owned this city now. The adrenaline began to flow, the thought of having that kind of control was intoxicating in a sick way.”
He wrote about the first soldier he saw killed in action, who had burned to death:
“What was left of his skeleton was hanging out of the driver-side door, his helmet a different color possibly fused to his skull and his IBA and plates which made up his torso, or what was left of it. That image still haunts me, it changed me. . . . I don’t know how many others saw that as we turned our trucks around but all I wanted was death and violence from then on. . . . To me this is where I lost my old self.”
He wrote about being home:
“I try so hard to be polite to everyone but I don’t know how much longer I can do it. I am trying to let this anger out bit by bit but it’s like holding up a dam with my mind, letting bit by bit out to keep it from going over the edge or breaking all together. Is there no medium, have I gone past that point where there is a safe way to get all this out without losing control? I am beginning to feel not. I feel it’s gonna happen soon. It’s just a matter of who says the wrong thing at the right time.”
He wrote about a nightmare:
“The anti-nightmare meds are not working. I was on a patrol last night and we entered a school, same as one from our deployment, but as we were clearing the school I went into an all-girl class and in real life they just screamed but in my dream they screamed and I opened fire, killing the whole class. What that is about I do not know. I am angry I have these dreams, I am angry they don’t stop. I miss my pleasant dreams of my past.”
He started to write about another nightmare, but he didn’t finish. Two weeks had passed, and he had made it past Level I, past Level II, and arrived at Level III. He could wear shoes with laces. He could shave unsupervised and go to the Loaf ’N Jug.
What he had written so far:
“What the f%#k is going on in my mind? Last night I was sitting in bed and looked across the room to a chair in my room and there was a young girl covered in blood. What happened after that I don’t remember. I was told a full-scale panic attack. This is not the first time I have seen dead bodies. For a while I used to find dead Iraqis floating in my bathtub. Why they were in the bathtub I will never know.
“i feel so f%#king violent right now.”
Suicide Rates During and After the Iraq and Afghanistan Wars
From October 7, 2001, to the end of December 2005, 144 veterans took their own lives. Of this number, twenty-four percent, or 35 vets, served in the Reserves, while 41 served in the National Guard. Sixty-eight of the 144 were active military/regular Army.
The New York Times reported on June 8, 2012, “The suicide rate among the nation’s active-duty military personnel has spiked this year, eclipsing the number of troops dying in battle and on pace to set a record annual high since the start of the wars in Iraq and Afghanistan more than a decade ago, the Pentagon said Friday.” This means that in the face of a troop withdrawal, the military must increase its efforts to assist our veterans with mental health, drug and alcohol, as well as financial counseling.
As of June 2012, 154 members of the active-duty military have committed suicide, an 18% increase, a rate of almost one a day. One hundred military members killed themselves last year (2014). One hundred twenty-three dying in 2010, and 133 in 2009.
Since 2001, more veterans have committed suicide than have died in combat operations in Iraq and Afghanistan, according to the Department of Veterans Affairs. That’s just one of many heartbreaking statistics found in “Crisis Hotline: Veterans Press 1,” a new HBO documentary that profiles the people working behind the scenes to help veterans and active-duty military members in their darkest hours.
“Veterans now account for 20 percent of suicides in the U.S., with the youngest (24 and under) taking their lives at four times the rate for other veteran age groups.
• US Army – 182 suicides
• US Marines Corps – 48 suicides
• US Navy – 60 suicides
• US Air Force – 59 suicides
According to their 2023 National Veteran Suicide Prevention Annual Report – based on data from 2021 – veteran suicide rates increased by 11.6% from 2020. On average, according to the VA, more than 17 veterans take their own lives each day.
Kimberly Hefling of the AP reports that “More than half of veterans who took their own lives after returning from Iraq or Afghanistan were members of the National Guard or Reserves.” Helfling’s information came from new government data and prompted activists to call for a closer examination of the problem. A Department of Veterans Affairs analysis of deaths among veterans of both wars found that Guard or Reserve members accounted for “53 percent of the veteran suicides from 2001, when the war in Afghanistan began, through the end of 2005.”
According to VA data, there were 6,392 veteran suicides from 2020-2021. This period saw the largest single year increase in veteran suicides, and veteran suicide is now the number two cause of death by veterans under the age of 45.
This number is likely much higher. The VA gets its numbers reported by county authorities throughout the country. This method failed to identify veterans about 18% of the time. The VA data also doesn’t include deaths aligned with self-harm, predominantly overdose deaths. According to an ongoing study by America’s Warrior Partnership, the actual number could be even higher with all the other data taken into account.
Family members and suicide
Reporter Ashley Fantz filed the following story for CNN, entitled “The Uncounted. The Spouse.” This story is about statistics seldom reported by the media. No one is keeping a count of the family members who have committed suicide due to loved ones KIA from the battles in Iraq212 and Afghanistan. Liz and her husband, Brian, have lived with his multiple deployments and single-parent home since 2003. Both Liz and Brian have paid a heavy price for serving our country.
Fantz writes,
In a hope chest at her home on Camp Pendleton in California, she kept a memento of her nomination as 2011’s Military Spouse of the Year. It was a huge honor in her world. “The nomination itself is an award for me,” she told a local news reporter at the time. “It takes qualities of strength and adaptability to thrive within the military spouse lifestyle.”
Liz Snell was very convincing. There was nothing she worked harder at than hiding the truth. Deployment after deployment, all the pressure, and fear, and weight of obligation had worn her down. The urge to make it stop consumed her. One afternoon, she walked into her bedroom closet with a plan.
Six years later, she remembers it as a dream: Standing outside of herself, she watched her hands as they tied a rope into a noose and slipped it over her head.
Several years ago, Deborah Mullen, wife of Admiral Mike Mullen, the then chairman of the Joint Chiefs of Staff, spoke at a Defense Department health care summit. Mrs. Mullen was attempting to call attention to the number of family members who were taking their lives due to losing family members in combat. The Army leaders with whom she was meeting knew of a total of nine relatives who had committed suicide in 2009. But when Deborah asked if the family members knew the numbers for those who had also committed suicide, Deborah was shocked at their answer. “I was stunned when I was told that there were too many to track,” she told the crowd. “If that number is that large just in the Army, we don't have an idea of the scope of the problem.”
According to their 2023 National Veteran Suicide Prevention Annual Report – based on data from 2021 – veteran suicide rates increased by 11.6% from 2020. On average, according to the VA, more than 17 veterans take their own lives each day.
• Why did Army wife Faye Vick take her life in 2006? The 36-year-old placed her baby and 2-year-old in the backseat of her car, the Raleigh News & Observer reported and asphyxiated them all.
• Could anything have helped Cassy Walton, wife of Iraq veteran Nils Andersson? He killed himself outside his Texas home in 2007. Just days later, she shot herself wearing her husband's dog tags and fatigue jacket.
• What made Monique Lingenfelter, the wife of a sergeant assigned to a special operations unit, barricade herself in her home near Fort Bragg, North Carolina, in 2009? Police tried for hours over a PA system to persuade the pregnant Army wife to come out. She killed herself, and her baby also died.
• What was going through Sheena Griffin’s mind in April 2010? While her husband was stationed at Fort Hood preparing to deploy to Afghanistan, Griffin told him that she wanted to kill herself and their 8-and 9-year-old sons. He called authorities. When police arrived at the family home, they found it engulfed in flames, and the mother and boys were shot dead.
Treatment
Wolfe, Keane, and Young have made several suggestions as to treatment for Gulf War vets. The scope of the veteran’s traumatic experiences needs attention paid to it. Clinicians must focus on a veteran’s pre-military as well as post-military stressors. Suppose a veteran had a history of abuse or trauma before service. In that case, exposure to severe stressors during combat could contribute significantly to the development of P.T.S.D. in the war zone and post-military separation. This exposure described my situation.
Finally, recognition and referral for assessment of the broad range of physical health concerns and complaints that may be reported by returning Veterans are important. Mental health providers must remember that increased health symptom reporting is unlikely to be exclusively psychogenic in origin.
Since the end of the Vietnam War and into the 1980s, combat traumatic stress became a common subject of writers when they first coined P.T.S.D. Vietnam veterans have assisted in reducing the symptoms, teaching better processing skills and creating beneficial medications.
Some doctors have taken into consideration the role of the family in the life of veterans, such as:
• Focus communication around patients’ concerns
• Organize information coherently
• Give risks as numbers
• Acknowledge scientific uncertainty
• Use universally understood language
• Focus on relieving symptoms
Once again, the U.S. government, which could do so much more, has become part of the problem. Note the following internet headlines: "Rep. Crow asks for answers on ‘troubling’ reported issues at Aurora VA hospital."
U.S. Rep. Jason Crow on Friday sent a letter to leadership in the U.S. Department of Veterans Affairs asking for further information on issues faced by veterans seeking care at the Rocky Mountain Regional Veterans Association Medical Center in Aurora.
The letter to VA Under Secretary of Health Dr. Shereef Elnahal comes one month after reporting from the Denver Post revealed the RMVA hospital prosthetics department canceled orders for veterans still in need in order to clear backlogs.
“I remain committed to ensuring not only the veterans in our community, but those who travel to this facility, receive the care they deserve,” Crow said in the letter. “There is a sacred promise in America that if you step up to serve, the nation will be there for you when you take off the uniform.”
Other “troubling information” cited by Crow in his letter relates to the VA’s Eastern Colorado Health Care System. Issues included:
staffing shortages
low morale
Scott Bronstein and Drew Griffin of CNN reported in April 23, 2014, "A fatal wait: Veterans languish and die on a VA hospital’s secret list."
The secret list was part of an elaborate scheme designed by Veterans Affairs managers in Phoenix who were trying to hide that 1,400 to 1,600 sick veterans were forced to wait months to see a doctor, according to a recently retired top VA doctor and several high-level sources.
Fox News reported, "These veterans served our country, now they say the VA is taking away their doctors."
Some years ago, his (Michael Cohen's) wife begged him to get help from the local Veterans Affairs medical facility in West Palm Beach, Florida. Cohen said he tried, but after many years and multiple VA therapists who could not see him on a regular basis, he decided to pay out-of-pocket for private care. He would like the VA to pay for his therapy through community care — a program designed for eligible veterans to receive care from a community provider when the VA cannot provide the care needed.
There is also this headline, “V.A. insults veteran treated for P.T.S.D. with phony address.” Sixty-four-year-old Gabriel Florido, a decorated Marine Lance Corporal who served in Vietnam, currently suffering from P.T.S.D., waited a year to receive his medication. The reason, according to Fox News, was that someone in the V.A. changed his address in the database “labeled address as ‘Coo Coo Lane.’” Florido now goes to a non-V.A. facility for treatment. Florido said in an interview with Fox News when asked how he felt, “I felt like someone spit in my face.” The Omaha, NE, V.A. facility has not apologized to Mr. Florido.






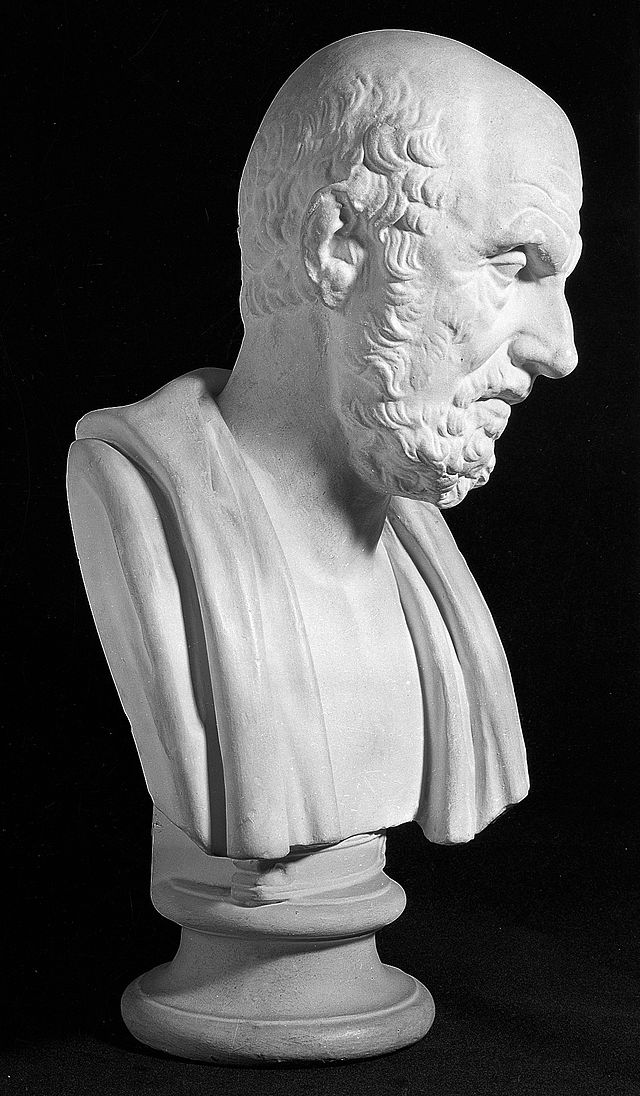





































Comments